What Is PTSD? Symptoms and Triggers You Should Know
Introduction
Post-Traumatic Stress Disorder (PTSD) is one of the most misunderstood mental health conditions—often associated only with war veterans or victims of severe violence. But in reality, PTSD can affect anyone who has experienced overwhelming or terrifying events that left deep emotional imprints.
This article dives into what PTSD truly is, how it manifests in everyday life, and what kinds of triggers can reignite its symptoms. Understanding these aspects is essential not only for those living with PTSD but also for loved ones, friends, and caregivers seeking to offer meaningful support.
Looking for supplements for This? Click here.
🌪️ Understanding PTSD: More Than Just “After a Trauma”

PTSD stands for Post-Traumatic Stress Disorder, a mental health condition that develops after a person experiences or witnesses a traumatic event. Such events may include physical assault, sexual abuse, natural disasters, car accidents, combat, or the sudden loss of a loved one. But trauma isn’t defined solely by the event itself—it’s about how the person’s mind and body process it.
When the brain experiences something terrifying or overwhelming, it activates a survival mechanism. Adrenaline surges. The heart races. Cortisol rises. The body goes into fight, flight, freeze, or fawn mode. This response is protective in the moment—but for some people, it doesn’t shut off once the danger is over.
Their nervous system remains “stuck” in hyper-alert mode, scanning for danger long after the event has passed. Over time, this can lead to intrusive memories, flashbacks, nightmares, and emotional detachment—all hallmarks of PTSD.
⚡ The Science Behind PTSD: When the Brain Can’t Move On
To understand PTSD, it helps to look at what happens in the brain after trauma.
The Amygdala – The Alarm System
The amygdala is responsible for detecting threats. During trauma, it becomes hyperactive, signaling “danger” even when none exists later on.
The Hippocampus – The Memory Organizer
This part of the brain helps distinguish between past and present experiences. In PTSD, the hippocampus becomes underactive, making it harder to recognize that the danger is no longer happening.
The Prefrontal Cortex – The Rational Brain
The prefrontal cortex normally calms the amygdala. But after trauma, it loses some of its control, which is why logical reasoning (“I’m safe now”) doesn’t always quiet fear or panic.
Together, these imbalances create a cycle of hypervigilance, intrusive thoughts, and emotional dysregulation that define PTSD.
💔 Common Causes of PTSD
Not everyone exposed to trauma develops PTSD. Genetic, psychological, and environmental factors all play a role. The following types of trauma are among the most common causes:
Physical or Sexual Assault – Survivors often relive the experience through flashbacks and fear of re-exposure.
War and Combat – Soldiers may experience hypervigilance, nightmares, and emotional numbness.
Accidents and Natural Disasters – Sudden, life-threatening events can imprint terror and helplessness.
Emotional or Psychological Abuse – Repeated emotional trauma, gaslighting, or humiliation can be just as damaging as physical trauma.
Childhood Neglect or Violence – Complex trauma (C-PTSD) can form when unsafe environments persist over years, altering the nervous system’s development.
Medical Emergencies or Chronic Illness – Extended hospitalizations, surgeries, or serious diagnoses can also trigger PTSD responses.
⚠️ Symptoms of PTSD: How It Shows Up in Everyday Life
PTSD doesn’t always look like dramatic flashbacks. It often hides beneath the surface—appearing as irritability, anxiety, emotional detachment, or exhaustion. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), PTSD symptoms fall into four main categories:
Intrusion Symptoms
These are the unwanted reminders of trauma that invade the present moment.
Flashbacks: Vivid re-experiencing of the event as if it’s happening again.
Nightmares: Disturbing dreams that echo the traumatic experience.
Intrusive thoughts or images: Sudden, distressing memories that feel uncontrollable.
Emotional reactivity: Intense distress when exposed to reminders of the trauma (like certain smells, sounds, or locations).
Intrusive symptoms make it difficult to relax because the mind keeps reliving the past.
Avoidance Symptoms
People with PTSD often go to great lengths to avoid reminders of what happened.
Avoiding places, people, or activities associated with the trauma.
Numbing emotions or disconnecting from feelings altogether.
Suppressing memories or refusing to talk about the event.
Avoidance may offer short-term relief but often reinforces PTSD over time because the brain never learns that the world can be safe again.
Negative Changes in Thinking and Mood
PTSD reshapes how someone views themselves and the world.
Persistent guilt or shame (“It was my fault,” “I should have done something”).
Loss of interest in activities once enjoyed.
Feeling detached from loved ones or emotionally flat.
Negative beliefs like “I can’t trust anyone” or “The world isn’t safe.”
These beliefs aren’t signs of weakness—they’re the mind’s attempt to make sense of trauma.
Hyperarousal and Reactivity
The body remains on high alert, as if danger is always near.
Insomnia or restless sleep.
Irritability or anger outbursts.
Difficulty concentrating.
Hypervigilance (always scanning for threats).
Startle response (jumpiness at loud noises).
This constant activation can exhaust the nervous system, leading to burnout and physical symptoms like muscle tension, rapid heartbeat, and headaches.
💭 Emotional and Physical Impact of PTSD
PTSD doesn’t just affect emotions—it impacts the entire body. Chronic stress hormones like cortisol and adrenaline remain elevated, affecting immune function, digestion, and even cardiovascular health.
Emotionally, PTSD can create feelings of shame, isolation, or disconnection. Many people feel trapped between wanting to forget and being unable to stop remembering. Relationships may suffer as partners misinterpret withdrawal or anger as rejection.
Some people with PTSD develop secondary conditions, including:
Depression
Anxiety or panic attacks
Substance abuse (to numb the pain)
Chronic fatigue or pain syndromes
Dissociation (feeling disconnected from oneself or reality)
PTSD is not “just in your head.” It’s a full-body experience of survival mode that needs to be treated compassionately and holistically.
Looking for online therapy ? Click Here.
🔥 Common PTSD Triggers
A trigger is anything—internal or external—that reminds a person of the trauma and reignites the body’s stress response.
Triggers can be obvious or subtle, and often they are sensory, emotional, or situational.
Sensory Triggers
Smells (perfume, smoke, alcohol, disinfectant)
Sounds (sirens, yelling, fireworks)
Visuals (certain lighting, environments, or objects)
Physical sensations (touch, pressure, or temperature)
Emotional Triggers
Feeling powerless or trapped
Experiencing rejection or abandonment
Arguments, anger, or confrontation
Witnessing another person’s distress
Situational Triggers
Returning to places where trauma occurred
Watching violent movies or news coverage
Being in crowds or unfamiliar settings
Anniversaries of the traumatic event
When a trigger occurs, the brain’s amygdala floods the body with stress hormones, causing a fight-or-flight reaction—even though the person is technically safe. That’s why triggers can feel so overwhelming and hard to control.
🌙 Complex PTSD (C-PTSD): When Trauma Is Repeated or Prolonged
While traditional PTSD often results from a single event, Complex PTSD (C-PTSD) develops after long-term exposure to trauma—like childhood neglect, domestic violence, or captivity.
C-PTSD shares many symptoms with PTSD but includes deeper emotional wounds such as:
Difficulty trusting others
Deep-seated shame or worthlessness
Fear of abandonment
Chronic dissociation
Emotional flashbacks (reliving the feelings, not the event itself)
C-PTSD requires gentle, long-term healing approaches that rebuild self-trust and safety.
🧘 The Nervous System and PTSD: Why the Body Remembers

Renowned trauma expert Dr. Bessel van der Kolk, in The Body Keeps the Score, emphasizes that trauma is stored in the body as much as in the mind. The nervous system “remembers” what happened through physical sensations—tightness, trembling, or sudden freezing—long after the conscious mind tries to forget.
When triggered, the body reacts before the rational brain even processes what’s happening. This explains why someone might suddenly dissociate, panic, or feel sick to their stomach in certain situations.
Healing therefore requires bottom-up approaches—techniques that calm the body before working through thoughts. This can include breathwork, yoga, grounding exercises, EMDR (Eye Movement Desensitization and Reprocessing), or somatic therapy.
🩹 How PTSD Is Diagnosed
A PTSD diagnosis is typically made by a mental health professional using the DSM-5 criteria, which requires that symptoms persist for at least one month after a traumatic event.
Diagnosis involves a thorough evaluation of:
The nature of the trauma (direct, witnessed, or learned about).
The presence of intrusive, avoidance, and arousal symptoms.
The impact on daily functioning (work, relationships, health).
It’s important to note that acute stress disorder (ASD) may occur within the first month after trauma. If symptoms persist beyond that, the diagnosis may shift to PTSD.
🌼 Treatment Options for PTSD
PTSD is treatable—but healing isn’t about erasing memories; it’s about retraining the body and mind to feel safe again.
Trauma-Focused Therapy
Evidence-based approaches like Cognitive Behavioral Therapy (CBT) and Prolonged Exposure Therapy help individuals face and reprocess their traumatic memories safely.
Looking for online therapy ? Click Here.
EMDR (Eye Movement Desensitization and Reprocessing)
This therapy uses guided eye movements to help rewire how traumatic memories are stored in the brain, reducing emotional charge and distress.
Somatic and Body-Based Therapies
Somatic Experiencing, trauma-informed yoga, or breathwork help regulate the nervous system and release trauma stored in the body.
Medication
Antidepressants (like SSRIs) may be prescribed to manage anxiety, depression, or hyperarousal. They’re not cures, but can create space for therapy to work more effectively.
Mindfulness and Meditation
Practices that cultivate present-moment awareness—like mindfulness meditation—help reduce hypervigilance and improve emotional regulation.
Support Groups and Peer Connection
Sharing experiences with others who understand trauma can reduce isolation and provide validation.
🧠 Coping Strategies and Daily Management
Healing from PTSD takes time and consistency. Here are ways to manage symptoms day to day:
Grounding Techniques: Focus on sensory experiences to anchor yourself in the present—like touching textured objects, noticing colors, or feeling your breath.
Journaling: Writing about emotions and triggers helps you identify patterns and express suppressed feelings safely.
Breathwork: Slow, deep breathing activates the parasympathetic nervous system, reducing panic and anxiety.
Want to try Breathwork? Click Here.
Movement: Gentle exercise like yoga, walking, or stretching releases built-up energy and improves mood.
Safe Space Visualization: Imagine a calming place where you feel completely secure. This can help soothe flashbacks or panic attacks.
Routine: Consistent daily rhythms—sleep, meals, and relaxation—rebuild a sense of stability after chaos.
🫶 Supporting Someone with PTSD
If you have a loved one with PTSD, compassion is the most powerful tool you can offer.
Do:
Listen without judgment or trying to “fix” them.
Encourage professional support.
Create an environment of safety and predictability.
Learn about triggers so you can avoid or manage them together.
Don’t:
Pressure them to “move on” or “get over it.”
Minimize their trauma.
Take their withdrawal or anger personally—it’s often a symptom, not rejection.
Healing requires patience and empathy from both sides.
🌈 Living Beyond PTSD: Hope and Healing
PTSD doesn’t define you—it’s a response your body created to survive something unbearable. With the right support, you can rewire your brain, calm your nervous system, and reclaim your sense of safety and self.
Recovery isn’t linear. Some days may feel calm, while others bring unexpected triggers. But with therapy, grounding practices, and social connection, the intensity of symptoms gradually fades. The nervous system learns safety again. The body learns peace.
People who heal from PTSD often describe gaining deep emotional insight, empathy, and inner strength—transforming survival into growth. You are not broken. You are a survivor whose nervous system is learning how to thrive again. 🌿
🧾 References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 2013.
van der Kolk, Bessel A. The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. Viking, 2014.
Yehuda R, et al. “Post-traumatic stress disorder.” Nature Reviews Disease Primers. 2015.
Shalev AY, et al. “Post-traumatic stress disorder.” New England Journal of Medicine. 2017.
Foa EB, et al. “Effective treatments for PTSD: Practice guidelines.” Guilford Press. 2009.
Bremner JD. “Traumatic stress: Effects on the brain.” Dialogues Clin Neurosci. 2006.
Ogden P, Fisher J. Sensorimotor Psychotherapy: Interventions for Trauma and Attachment. 2015.
Herman JL. Trauma and Recovery: The Aftermath of Violence—from Domestic Abuse to Political Terror. Basic Books, 1992.
Cloitre M, et al. “Complex PTSD: A new diagnosis in ICD-11.” World Psychiatry. 2018.
National Center for PTSD. “Understanding PTSD and Recovery.” U.S. Department of Veterans Affairs, 2022.
Related Posts
-

Magnesium and PTSD: Calming the Nervous System
Magnesium is one of the body’s most powerful natural stress relievers. 🌿 Learn how this essential mineral helps calm the nervous system, lower cortisol, ease anxiety, and support better sleep—making it a key ally for anyone recovering from trauma or PTSD.
-
Omega-3s for PTSD: Supporting Brain Health and Emotional Balance
Omega-3s play a vital role in calming the brain and restoring balance after trauma. 🌊 Discover how these essential fatty acids support PTSD recovery by reducing inflammation, balancing neurotransmitters, improving sleep, and promoting emotional resilience—helping your brain heal from the inside out.
-
Ashwagandha and PTSD: Reducing Stress and Anxiety Naturally
Ashwagandha offers a natural path to stress and trauma recovery by calming the body’s stress response and restoring hormonal balance. 🌿 Learn how this powerful adaptogen can lower cortisol, ease anxiety, improve sleep, and support emotional resilience for those healing from PTSD.
-

GABA and PTSD: Supporting Calm After Trauma
Therapy helps the brain rewire after trauma, restoring safety and self-trust. 🛋️ Discover how modern therapeutic approaches—like EMDR, CBT, and somatic therapy—help regulate the nervous system, calm intrusive memories, and rebuild emotional resilience for people recovering from PTSD and chronic stress.
-

PTSD and Brain Chemistry: How Nutrition and Supplements Play a Role
PTSD isn’t just psychological—it’s deeply biological. 🧠 Learn how trauma reshapes brain chemistry and how nutrition, omega-3s, magnesium, B vitamins, and adaptogens can help rebalance neurotransmitters, reduce inflammation, and support emotional recovery from the inside out.
-

Can Supplements Support Trauma Recovery? Evidence & Insights
Can nutrients like Vitamin D and Zinc really support trauma recovery? 🌞 These two essential micronutrients play powerful roles in immune balance, inflammation control, and hormonal stability—all key systems disrupted by chronic stress and trauma. Learn how replenishing them can help restore strength and emotional resilience.
-
The Role of Cortisol in PTSD and How Supplements May Help
Your adrenal glands play a vital role in how your body responds to stress—but when they’re overworked, fatigue and anxiety can follow. 🌿 Learn how to support adrenal health naturally with nutrients, adaptogens like ashwagandha and rhodiola, and lifestyle habits that restore hormonal balance and steady energy.
-

Creating a Daily Supplement Stack for Stress and Cortisol Management: A Science-Based Guide
Building a daily supplement stack for stress and cortisol management can help restore balance, focus, and calm in your life. 🌿 Learn how adaptogens, magnesium, omega-3s, and other key nutrients support your body’s natural stress response from morning to night—so you can feel grounded, energized, and resilient every day.
-

How Meditation and Supplements Work Together to Reduce Cortisol: A Complete Guide to Calming the Mind and Body
Meditation and supplements can work hand in hand to naturally reduce cortisol, your body’s main stress hormone. 🌿 Learn how mindfulness practices, adaptogenic herbs, and nutrient support like magnesium, omega-3s, and B vitamins create a powerful synergy for calm, focus, and emotional balance—backed by science and daily rituals that truly reset your stress response.
-

Cortisol Reset: Supplements + Daily Habits That Work
-
The Role of Adaptogens in Balancing Stress Hormones
Adaptogens work at the root of stress — your nervous system. 🌿 Learn how these powerful herbs help regulate cortisol, calm your nerves, and restore balance between energy and relaxation. ✨
-

Cortisol and Caffeine: How Much Is Too Much?
Caffeine can boost energy and focus — but too much can overstimulate your stress hormones. ☕ Learn how caffeine affects cortisol, energy levels, and mood, and discover how to find the perfect balance for lasting calm and clarity. 🌿
-
Antioxidants for Stress Management and Cortisol Control
When stress overwhelms your body, antioxidants come to the rescue. 🌿 Learn how vitamin C, CoQ10, and other natural compounds help reduce oxidative stress, regulate cortisol, and restore calm energy from within. ✨
-

Cortisol and Gut Health: How Probiotics May Help
Chronic stress doesn’t just affect your mind — it changes your gut. 🌿 Learn how cortisol disrupts the microbiome and how probiotics can help restore balance, improve digestion, and calm your stress response naturally. ✨
-

Vitamin D and Cortisol: Supporting Immune Balance
Vitamin D does more than strengthen bones — it helps regulate cortisol and support immune balance. 🌞 Learn how this essential hormone-like nutrient restores calm, improves mood, and strengthens your body’s natural stress defenses. 🌿
-

Omega-3s and Cortisol: Fighting Inflammation Naturally
Omega-3s are more than heart-healthy fats — they’re natural cortisol regulators. 🌿 Learn how EPA and DHA help reduce chronic inflammation, calm the nervous system, and support stress recovery from the inside out. ✨
-

High Cortisol and Belly Fat: Can Supplements Help?
Chronic stress can make belly fat harder to lose — but supplements like ashwagandha, magnesium, and omega-3s may help restore cortisol balance. 🌿 Learn how science-backed nutrients support fat metabolism, calm your stress response, and bring your body back into harmony. ✨
-

How Ginseng Can Support Energy and Cortisol Balance
Ginseng is one of nature’s most powerful adaptogens, helping your body handle stress without burning out. 🌿 Learn how this ancient root supports balanced cortisol, steady energy, and sharper focus — restoring vitality naturally and sustainably. ✨
-

Taurine and Cortisol: Supporting Focus Under Stress
When cortisol surges, focus fades — but taurine helps restore balance. 🌿 Learn how this powerful amino acid calms your nervous system, regulates stress hormones, and sharpens concentration without jitters or fatigue. ✨
-
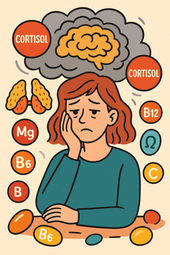
The Link Between Cortisol, Brain Fog, and Nutrient Deficiencies
When brain fog sets in, it’s not just in your head — it’s in your hormones. 🌿 Discover how cortisol imbalance and nutrient deficiencies like low magnesium, B vitamins, and omega-3s can cloud your focus and how restoring balance brings back mental clarity and calm. ✨
-

B Vitamins for Stress, Energy, and Cortisol Regulation
B vitamins are the foundation of stress resilience and steady energy. 🌿 Learn how this essential group of nutrients helps regulate cortisol, restore focus, and keep your nervous system calm — giving you balance from the inside out. ✨
-

Cortisol Imbalance and Chronic Fatigue: Can Supplements Help?
When chronic stress keeps cortisol high, fatigue and brain fog follow. 🌿 Learn how to rebalance your stress hormones naturally with calming nutrients, adaptogens, and lifestyle rituals that restore energy, focus, and inner peace. ✨
-

Adaptogen Stacks for Better Sleep and Lower Stress Hormones
Adaptogens can help your body recover from stress and sleep better by regulating key hormones like cortisol and adrenaline. 🌿 Learn how adaptogen stacks work to restore balance, calm the mind, and rebuild resilience — so you can rest deeply and wake renewed. ✨
-

Phosphatidylserine for Nighttime Cortisol Control
When stress hormones stay high at night, deep rest becomes impossible. 🌙 Discover how phosphatidylserine helps calm the brain, reduce nighttime cortisol, and restore healthy sleep rhythms — so you can wake up peaceful, clear, and recharged. ✨
-

Magnesium for Stress Relief and Cortisol Reduction
Magnesium is one of the most powerful natural tools for stress relief. 🌿 This essential mineral calms your nervous system, lowers cortisol, and helps your body recover from chronic tension. Learn how magnesium replenishes balance, improves sleep, and restores inner peace — naturally. ✨
-

Supplements to Improve Sleep by Balancing Cortisol
When cortisol stays high at night, sleep becomes a struggle. 🌙 Discover natural supplements that calm the nervous system, lower stress hormones, and restore your body’s natural rhythm. From magnesium and ashwagandha to L-theanine and phosphatidylserine, learn how to build deeper, more restorative rest. 🌿
-

Cortisol and Sleep: Why Stress Keeps You Awake
When stress keeps your body in fight-or-flight mode, cortisol refuses to calm down — and sleep becomes impossible. 🌙 Learn how elevated cortisol disrupts your circadian rhythm, suppresses melatonin, and turns restless nights into exhaustion. Discover how to restore balance and reclaim deep rest. ✨
-

L-Theanine for Cortisol Balance and Anxiety Relief
L-Theanine — the calming amino acid from green tea — helps quiet the mind and balance cortisol, the body’s key stress hormone. 🌿 Learn how it promotes calm focus, eases anxiety, and supports deep rest without sedation, backed by modern research and centuries of tradition. ✨
-

Rhodiola Rosea and Stress Resilience: A Natural Cortisol Regulator
Rhodiola rosea is one of nature’s most powerful tools for resilience. 🌿 This Arctic root helps balance cortisol, fight fatigue, and sharpen focus — keeping you calm yet energized even under stress. Discover the science behind Rhodiola’s adaptogenic power and how it helps your body thrive under pressure. ✨
-

Ashwagandha for Cortisol Balance: What the Science Says
Ashwagandha helps your body recover from chronic stress by calming the adrenal system and balancing cortisol — your key stress hormone. 🌿 Learn what science says about this powerful adaptogen, how it restores energy and focus, and why it’s one of nature’s most effective tools for modern stress relief. ✨
-

Supplements That Naturally Lower Cortisol Levels
When cortisol levels calm, your energy transforms — no more crashes or jitters, just steady focus and inner peace. 🌿 Learn which natural supplements and habits lower stress hormones, boost calm energy, and help your body thrive with balance instead of burnout. ✨
-

What Is Cortisol Imbalance? Symptoms You Shouldn’t Ignore
Cortisol — your body’s main stress hormone — keeps you alert and energized, but when it’s out of balance, it can drain your health. 🌿 Learn the signs of cortisol imbalance, from fatigue and anxiety to sleep disruption and stubborn weight gain, and discover how to restore calm, energy, and hormonal harmony naturally. ✨
-

The Best Daily Multivitamins for Menopausal Women
Menopause brings new nutritional needs that your old vitamin routine may no longer meet. 🌿 Discover how the right daily multivitamin can boost energy, balance mood, support bone and heart health, and keep your skin glowing. Learn which nutrients truly matter — from vitamin D to magnesium and B12 — to feel strong and vibrant every day. ✨
-

Antioxidants and Menopause: Fighting Inflammation Naturally
During menopause, oxidative stress and inflammation can quietly accelerate aging, fatigue, and skin changes. 🌿 Learn how antioxidants — from vitamins C and E to polyphenols in berries and green tea — help neutralize free radicals, reduce inflammation, and restore balance naturally. Discover the science of radiant, resilient aging. ✨
-

How CoQ10 Supports Heart Health After Menopause
After menopause, heart health becomes more important than ever. ❤️ Discover how CoQ10 — your body’s natural energy molecule — supports cardiovascular strength, restores vitality, and protects against oxidative stress. Learn how this essential nutrient helps keep your heart energized, balanced, and resilient through every stage of life. 🌿
-

Collagen Supplements for Skin and Joint Health Post-Menopause
After menopause, collagen loss affects both skin elasticity and joint comfort — but supplements can help rebuild from within. 🌸 Learn how collagen peptides, vitamin C, and other nutrients work together to restore firmness, reduce stiffness, and keep you glowing and mobile well into your next chapter. ✨
-

Calcium and Vitamin D: Protecting Bone Health in Menopause
Menopause brings hormonal changes that can weaken bones—but with the right nutrients, strength and stability can be rebuilt. 🦴 Learn how calcium and vitamin D work together to protect bone density, prevent fractures, and keep your body resilient. This guide explores nutrition, sunlight, and lifestyle habits that help your bones stay strong and vibrant for years to come. ☀️💪
-

Adaptogens for Energy and Resilience During Menopause
Feeling drained or emotionally scattered during menopause? 🌿 Discover how adaptogenic herbs like Ashwagandha, Rhodiola, and Ginseng can restore energy, balance cortisol, and build emotional resilience. Learn how these natural allies work with your body—not against it—to help you stay strong, focused, and calm through life’s hormonal changes. 🌸
-

Supplements That Help Beat Menopause Fatigue
Menopause fatigue can feel like more than tiredness—it’s a total energy crash. This guide explores how specific supplements, mindful breathwork, and therapy can help restore balance. Learn how nutrients like B vitamins, magnesium, and adaptogens rebuild your stamina, while breathwork and emotional healing calm your nervous system and bring vitality back to your days. 🌿✨
-

Herbal Blends for Menopausal Restlessness: Finding Calm in Transition
Herbal blends bring the wisdom of nature into moments of rest and renewal. Discover how soothing herbs like chamomile, lemon balm, and ashwagandha work together to calm menopausal restlessness, balance hormones, and invite deep relaxation. 🌿💫
-

Magnesium + Glycine for Deep Sleep During Menopause
Nutrients like magnesium, glycine, and B vitamins form the foundation for deep, restorative sleep during menopause. Discover how these natural compounds calm your nervous system, balance hormones, and help you wake up refreshed and recharged. 🌿💤
-

Melatonin and Menopause: Restoring Your Sleep Cycle
Nutrients are the foundation of hormone balance and energy. Learn how vitamins, minerals, and whole foods like greens, salmon, and berries nourish women’s bodies during menopause and beyond — restoring vitality, mood, and strength. 🌿🥗
-

How L-Theanine Helps With Menopausal Anxiety
Science continually deepens our understanding of the human body, from hormones to neurotransmitters. Discover how evidence-based research shapes modern wellness — bridging natural medicine, neuroscience, and hormone balance for healthier living. 🔬🌿
-

Can Ginkgo Biloba Improve Memory in Menopausal Women?
Hormone therapy can be a powerful tool for easing menopause symptoms and restoring balance. Learn how it works, the types available, and how to combine it safely with lifestyle and natural support for optimal well-being. 🌸💊
-

B Vitamins for Mental Clarity During Menopause
Nutrients are the foundation of mental and physical balance during menopause. Discover how vitamins, minerals, and whole foods like leafy greens, fish, nuts, and citrus can fuel energy, clarity, and calm while supporting hormonal health. 🌿✨
-

Mood Swings and Menopause: Natural Nutrient Support
Probiotics do more than support digestion — they help balance mood, hormones, and immunity too. Learn how a healthy gut microbiome can ease menopause symptoms, boost energy, and improve emotional resilience naturally. 🌿🦠
-

Brain Fog in Menopause: Supplements That May Help
Supplements can be powerful allies in restoring balance, energy, and focus—especially during menopause. Learn how nutrients like omega-3s, vitamin D, magnesium, and herbal adaptogens work together to support brain health, reduce stress, and promote lasting vitality. 🌿💊
-

Adaptogen Stacks for Reducing Night Sweats
Hormone detox isn’t about cleansing your body—it’s about restoring flow. Learn how the liver, gut, and endocrine systems work together to eliminate hormone buildup and how herbs like milk thistle, dandelion, and schisandra support balance, clarity, and natural vitality. 🌿💫
-

Cooling Menopause Symptoms with Herbal Support
Ashwagandha is one of nature’s most powerful adaptogens, helping women manage stress, sleep better, and balance hormones naturally. Discover how this ancient root supports calm energy, emotional resilience, and relief from menopause-related anxiety and fatigue. 🌿💫