Magnesium and PTSD: Calming the Nervous System
Introduction
Post-Traumatic Stress Disorder (PTSD) is a condition that leaves the mind and body in a constant state of alertness. Even after the traumatic event has ended, the body continues to act as though danger is still present. For many people, this means living with chronic anxiety, muscle tension, insomnia, and fatigue.
One of the most overlooked yet powerful tools for restoring calm in the body is magnesium—a mineral involved in more than 300 biochemical reactions, including those that regulate stress, sleep, and mood.
Magnesium deficiency is surprisingly common, especially in people exposed to chronic stress. For individuals with PTSD, replenishing magnesium can help soothe the nervous system, reduce anxiety, and support better emotional regulation.
This article explores how magnesium influences the brain, the stress response, and trauma recovery—and how supplementing it can help restore balance to both mind and body.
Looking for supplements for This? Click here.
🌪️ PTSD and the Hyperactive Nervous System

When someone experiences trauma, the brain’s alarm system—the amygdala—becomes hypersensitive. It keeps sending danger signals to the body, even when no real threat exists.
This activates the sympathetic nervous system (fight-or-flight mode), flooding the body with stress hormones like cortisol and adrenaline.
In a healthy system, the parasympathetic nervous system (rest-and-digest mode) eventually steps in to restore calm. But in PTSD, this switch often malfunctions. The body stays “on” almost all the time, leading to:
Anxiety and hypervigilance
Insomnia and restless sleep
Muscle tension and irritability
Digestive problems
Fatigue and adrenal burnout
Over time, this chronic activation depletes key minerals and nutrients—including magnesium—which the body burns through rapidly during stress.
🧬 Why Magnesium Matters for Stress and Trauma
Magnesium is often called the “relaxation mineral.” It plays a central role in regulating the nervous system, muscle function, and hormone balance.
When you’re deficient, the brain and body literally can’t relax.
Here’s how magnesium supports the systems affected by trauma:
Regulates the Stress Response (HPA Axis)
Magnesium helps control the hypothalamic-pituitary-adrenal (HPA) axis, which governs cortisol production. When magnesium levels are low, cortisol remains elevated for longer—keeping the body trapped in fight-or-flight mode.
Activates GABA Receptors
Magnesium enhances the activity of GABA (gamma-aminobutyric acid), a neurotransmitter that promotes calm. Low GABA is linked to anxiety, insomnia, and overstimulation—all common in PTSD.
Reduces Glutamate Excitotoxicity
Magnesium blocks NMDA (N-methyl-D-aspartate) receptors, preventing overactivation by glutamate—the brain’s primary excitatory neurotransmitter. Too much glutamate can cause anxiety, irritability, and even neuron damage.
Supports Serotonin and Dopamine Balance
Magnesium is essential for the synthesis and regulation of serotonin and dopamine, two neurotransmitters that govern mood and motivation.
Improves Sleep and Muscle Relaxation
By relaxing the nervous system and muscles, magnesium helps reduce nighttime restlessness and supports deep, restorative sleep—a crucial element of trauma recovery.
⚠️ The Link Between PTSD and Magnesium Deficiency
Research shows that chronic stress depletes magnesium through urine loss and cellular breakdown. When trauma becomes long-term, the body struggles to replenish it fast enough.
Symptoms of magnesium deficiency closely mirror those of PTSD:
Anxiety or panic
Restlessness and irritability
Insomnia
Muscle cramps or twitching
Fatigue and brain fog
Heart palpitations
In trauma survivors, this deficiency creates a vicious cycle: stress depletes magnesium, low magnesium worsens stress tolerance, and the nervous system becomes increasingly fragile.
Studies suggest that magnesium deficiency may even worsen fear conditioning—the process by which neutral events become associated with trauma. Replenishing magnesium helps “unlearn” these fear patterns by normalizing brain communication.
🌿 The Science: How Magnesium Calms the PTSD Brain
Let’s look deeper into how magnesium interacts with specific brain regions and chemical pathways affected by trauma.
The Amygdala (Fear Center)
Trauma makes the amygdala hyperactive, constantly scanning for threats. Magnesium calms this overactivity by increasing GABA and reducing glutamate signaling.
The Hippocampus (Memory and Context)
The hippocampus helps distinguish between past and present experiences. Chronic stress shrinks this region—but magnesium supports BDNF (Brain-Derived Neurotrophic Factor), a protein that promotes hippocampal growth and repair.
The Prefrontal Cortex (Reason and Regulation)
Magnesium strengthens the prefrontal cortex’s ability to regulate emotional responses, improving impulse control and rational thinking during stressful moments.
In short, magnesium helps rebuild the neural pathways that allow the brain to interpret the world safely again.
🩹 Magnesium and the Body: Beyond the Brain
The benefits of magnesium for trauma recovery extend throughout the body:
Reduces muscle tension and tightness often caused by chronic hyperarousal.
Supports heart rhythm by stabilizing electrical impulses in cardiac tissue.
Improves digestion by relaxing intestinal muscles and supporting healthy peristalsis.
Regulates blood sugar, preventing energy crashes that worsen anxiety.
Supports hormonal balance, including cortisol, estrogen, and testosterone—all impacted by trauma.
This full-body effect is why magnesium is sometimes called a “system-wide relaxant.”
🌸 Magnesium and Sleep in PTSD
Sleep disturbance is one of the most debilitating symptoms of PTSD. The mind races, the body stays tense, and nightmares or flashbacks prevent rest.
Magnesium helps regulate melatonin and GABA, two compounds essential for falling and staying asleep.
Clinical studies show that magnesium supplementation:
Increases total sleep time
Improves sleep onset (falling asleep faster)
Reduces nighttime awakenings
Decreases cortisol levels before bed
Better sleep leads to improved emotional regulation, memory processing, and immune resilience—all vital for trauma recovery.
🌿 Forms of Magnesium: Choosing the Right One
Not all magnesium supplements are created equal. Some forms absorb better and target different symptoms.
Magnesium Glycinate
Highly bioavailable and gentle on the stomach.
Best for calming anxiety, improving sleep, and reducing muscle tension.
Ideal for trauma recovery.
Magnesium Threonate
Crosses the blood-brain barrier effectively.
Enhances cognitive function, focus, and memory.
Great for those with brain fog or emotional detachment.
Magnesium Citrate
Supports digestion and relieves constipation.
Mildly energizing, suitable for daytime use.
Magnesium Malate
Combats fatigue and supports energy metabolism.
May help those with depression or chronic exhaustion.
Magnesium Chloride or Sulfate (Topical)
Absorbed through the skin via magnesium oils or Epsom salt baths.
Useful for localized muscle relaxation and stress relief before sleep.
For PTSD and anxiety, magnesium glycinate or threonate are usually the most effective choices.
Looking for supplements for This? Click here.
💊 Suggested Dosage
General calming support: 200–400 mg daily (elemental magnesium).
Sleep support: 200 mg magnesium glycinate 1–2 hours before bed.
Cognitive support: 100–200 mg magnesium threonate daily.
Always start low and increase gradually, as high doses can cause loose stools. Pair magnesium with food or take it in divided doses for better absorption.
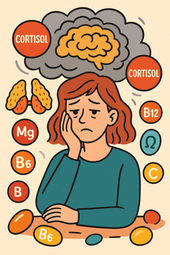
⚖️ Magnesium in Combination with Other Nutrients
Magnesium works synergistically with several other nutrients that support trauma recovery:
Vitamin B6: Enhances magnesium’s absorption and GABA synthesis.
Zinc: Regulates the stress response and hormone balance.
Vitamin D: Improves magnesium uptake in cells and supports mood stability.
Taurine: Works alongside magnesium to calm the nervous system.
Omega-3 fatty acids: Reduce inflammation and improve neural communication.
Together, these nutrients form a biochemical foundation for calm and emotional balance.
🌬️ Magnesium and the Vagus Nerve: The Body’s “Brake Pedal”
The vagus nerve is a key player in trauma recovery. It connects the brain to the heart, lungs, and gut, and governs the parasympathetic (rest-and-digest) system.
Magnesium enhances vagal tone by lowering heart rate, supporting relaxation, and improving gut-brain communication.
This can reduce symptoms like:
Shortness of breath or tight chest
Gut discomfort during stress
Emotional overwhelm
Practices like deep breathing, yoga, humming, or cold exposure—combined with adequate magnesium—can strengthen vagal function and retrain the nervous system to rest more easily.
🧘 Magnesium and Emotional Regulation
Many people with PTSD describe feeling “emotionally hijacked”—their body reacts before their mind can catch up.
This is a direct reflection of neurochemical imbalance. Magnesium helps restore emotional regulation by:
Lowering norepinephrine (adrenaline-like) activity.
Enhancing serotonin receptor sensitivity.
Supporting dopamine balance, preventing burnout and apathy.
The result is a smoother, steadier emotional baseline—less volatility, fewer anxiety spikes, and improved capacity to handle triggers.
🌿 Clinical Research on Magnesium and PTSD
While studies specifically on magnesium and PTSD are still emerging, related research on anxiety, depression, and stress disorders is extensive:
Tarleton et al. (2017): Magnesium supplementation significantly reduced anxiety scores within two weeks, with notable improvements in sleep and calmness.
Boyle et al. (2017): Found magnesium effective for mild-to-moderate depression and stress relief, especially in those with low baseline magnesium levels.
Serefko et al. (2013): Demonstrated magnesium’s antidepressant-like effects through GABA and serotonin modulation.
Rosanoff (2019): Identified magnesium deficiency as a “silent epidemic” that amplifies stress-related illnesses.
In PTSD, where chronic hyperarousal and sleep disturbance are central symptoms, magnesium’s effects on GABA and cortisol make it an ideal complementary therapy.
🌼 How to Integrate Magnesium into Trauma Recovery

Magnesium alone won’t heal PTSD—but it lays a biochemical foundation for healing.
Here’s how to integrate it into a broader recovery routine:
Combine with Therapy
Magnesium helps the nervous system stay calm, allowing you to process emotions during EMDR, CBT, or somatic therapy without feeling overwhelmed.
Support with Nutrition
Eat magnesium-rich foods daily:
Leafy greens (spinach, kale)
Avocados
Almonds, cashews, pumpkin seeds
Dark chocolate
Legumes and whole grains
Prioritize Sleep Hygiene
Use magnesium at night to improve rest. Create a wind-down routine: dim lights, deep breathing, herbal tea, and perhaps an Epsom salt bath.
Practice Nervous System Regulation
Complement magnesium with breathwork, yoga, grounding exercises, and mindfulness to activate the parasympathetic nervous system.
Want to try Breathwork? Click Here.
Stay Consistent
Magnesium works gradually—consistent use for 4–8 weeks yields the best results.
Looking for online therapy ? Click Here.
🧘 Sample Daily Routine for Magnesium and Nervous System Calm
Morning
Breakfast with avocado toast or a smoothie with spinach and banana.
100 mg magnesium malate or citrate (for energy).
15 minutes of sunlight or gentle stretching.
Afternoon
Balanced meal with greens, salmon, or lentils.
Deep breathing or grounding exercises for vagal activation.
Evening
200 mg magnesium glycinate 1 hour before bed.
Herbal tea (chamomile, lemon balm, or reishi).
Epsom salt bath or warm shower.
Journaling or gratitude reflection to calm racing thoughts.
This routine combines biochemical and emotional regulation—helping the body feel safe again.
🌙 Long-Term Benefits of Magnesium for PTSD
With consistent use, magnesium replenishment can transform the way your nervous system responds to stress.
Long-term benefits include:
Lower anxiety and panic frequency
Improved sleep and energy levels
Reduced irritability and emotional fatigue
Calmer digestion and heart rhythm
Greater emotional stability
By restoring cellular energy and neurotransmitter balance, magnesium helps the body finally relax after years of hyperactivation.
⚠️ Precautions and Contraindications
While magnesium is safe for most people, keep these tips in mind:
High doses can cause diarrhea; start slow.
Consult your doctor if you have kidney disease or use medications like diuretics or antibiotics.
Avoid taking magnesium at the exact same time as thyroid or antibiotic medication (wait at least 2 hours).
Magnesium is best taken with food or before bedtime for maximum absorption and relaxation.
💫 Healing Through Chemistry and Compassion
PTSD recovery is not about “controlling” your mind—it’s about teaching your body to feel safe again.
Magnesium gives your nervous system the biochemical stability it needs to support that process. When combined with therapy, mindfulness, and gentle self-care, it creates the internal conditions for healing.
As your magnesium stores rebuild, you may notice:
Your breathing slows.
Sleep comes easier.
Panic fades faster.
Your body feels lighter, more relaxed.
These are signs that your nervous system is remembering peace—and that’s one of the most hopeful milestones on the trauma recovery journey. 🌿
Looking for online therapy ? Click Here.
🧾 References
Tarleton EK, et al. “Effects of magnesium supplementation on anxiety and stress in adults.” PLoS One. 2017.
Boyle NB, et al. “The effects of magnesium supplementation on subjective anxiety.” Nutrients. 2017.
Serefko A, et al. “Magnesium in depression and anxiety: A review.” Pharmacol Rep. 2013.
Rosanoff A. “Magnesium’s role in stress and mental health.” Adv Nutr. 2019.
Blom EH, et al. “Magnesium and mood regulation.” Nutrients. 2018.
Yehuda R. “Cortisol and HPA-axis alterations in PTSD.” Psychoneuroendocrinology. 2015.
van der Kolk, Bessel A. The Body Keeps the Score. Viking, 2014.
Raison CL, Miller AH. “Inflammation and stress-related disorders.” Am J Psychiatry. 2013.
Eby GA, Eby KL. “Rapid recovery from major depression using magnesium treatment.” Med Hypotheses. 2006.
National Center for PTSD. “Managing Stress Responses.” U.S. Department of Veterans Affairs, 2022.
Related Posts
-
Omega-3s for PTSD: Supporting Brain Health and Emotional Balance
Omega-3s play a vital role in calming the brain and restoring balance after trauma. 🌊 Discover how these essential fatty acids support PTSD recovery by reducing inflammation, balancing neurotransmitters, improving sleep, and promoting emotional resilience—helping your brain heal from the inside out.
-
Ashwagandha and PTSD: Reducing Stress and Anxiety Naturally
Ashwagandha offers a natural path to stress and trauma recovery by calming the body’s stress response and restoring hormonal balance. 🌿 Learn how this powerful adaptogen can lower cortisol, ease anxiety, improve sleep, and support emotional resilience for those healing from PTSD.
-

GABA and PTSD: Supporting Calm After Trauma
Therapy helps the brain rewire after trauma, restoring safety and self-trust. 🛋️ Discover how modern therapeutic approaches—like EMDR, CBT, and somatic therapy—help regulate the nervous system, calm intrusive memories, and rebuild emotional resilience for people recovering from PTSD and chronic stress.
-

PTSD and Brain Chemistry: How Nutrition and Supplements Play a Role
PTSD isn’t just psychological—it’s deeply biological. 🧠 Learn how trauma reshapes brain chemistry and how nutrition, omega-3s, magnesium, B vitamins, and adaptogens can help rebalance neurotransmitters, reduce inflammation, and support emotional recovery from the inside out.
-

Can Supplements Support Trauma Recovery? Evidence & Insights
Can nutrients like Vitamin D and Zinc really support trauma recovery? 🌞 These two essential micronutrients play powerful roles in immune balance, inflammation control, and hormonal stability—all key systems disrupted by chronic stress and trauma. Learn how replenishing them can help restore strength and emotional resilience.
-
The Role of Cortisol in PTSD and How Supplements May Help
Your adrenal glands play a vital role in how your body responds to stress—but when they’re overworked, fatigue and anxiety can follow. 🌿 Learn how to support adrenal health naturally with nutrients, adaptogens like ashwagandha and rhodiola, and lifestyle habits that restore hormonal balance and steady energy.
-

What Is PTSD? Symptoms and Triggers You Should Know
Post-Traumatic Stress Disorder (PTSD) can affect anyone who has experienced deep emotional or physical trauma. 🌪️ Learn how PTSD develops, what symptoms to look for, and the triggers that reignite distress—plus how understanding your body’s response to trauma is the first step toward healing and recovery.
-

Creating a Daily Supplement Stack for Stress and Cortisol Management: A Science-Based Guide
Building a daily supplement stack for stress and cortisol management can help restore balance, focus, and calm in your life. 🌿 Learn how adaptogens, magnesium, omega-3s, and other key nutrients support your body’s natural stress response from morning to night—so you can feel grounded, energized, and resilient every day.
-

How Meditation and Supplements Work Together to Reduce Cortisol: A Complete Guide to Calming the Mind and Body
Meditation and supplements can work hand in hand to naturally reduce cortisol, your body’s main stress hormone. 🌿 Learn how mindfulness practices, adaptogenic herbs, and nutrient support like magnesium, omega-3s, and B vitamins create a powerful synergy for calm, focus, and emotional balance—backed by science and daily rituals that truly reset your stress response.
-

Cortisol Reset: Supplements + Daily Habits That Work
-
The Role of Adaptogens in Balancing Stress Hormones
Adaptogens work at the root of stress — your nervous system. 🌿 Learn how these powerful herbs help regulate cortisol, calm your nerves, and restore balance between energy and relaxation. ✨
-

Cortisol and Caffeine: How Much Is Too Much?
Caffeine can boost energy and focus — but too much can overstimulate your stress hormones. ☕ Learn how caffeine affects cortisol, energy levels, and mood, and discover how to find the perfect balance for lasting calm and clarity. 🌿
-
Antioxidants for Stress Management and Cortisol Control
When stress overwhelms your body, antioxidants come to the rescue. 🌿 Learn how vitamin C, CoQ10, and other natural compounds help reduce oxidative stress, regulate cortisol, and restore calm energy from within. ✨
-

Cortisol and Gut Health: How Probiotics May Help
Chronic stress doesn’t just affect your mind — it changes your gut. 🌿 Learn how cortisol disrupts the microbiome and how probiotics can help restore balance, improve digestion, and calm your stress response naturally. ✨
-

Vitamin D and Cortisol: Supporting Immune Balance
Vitamin D does more than strengthen bones — it helps regulate cortisol and support immune balance. 🌞 Learn how this essential hormone-like nutrient restores calm, improves mood, and strengthens your body’s natural stress defenses. 🌿
-

Omega-3s and Cortisol: Fighting Inflammation Naturally
Omega-3s are more than heart-healthy fats — they’re natural cortisol regulators. 🌿 Learn how EPA and DHA help reduce chronic inflammation, calm the nervous system, and support stress recovery from the inside out. ✨
-

High Cortisol and Belly Fat: Can Supplements Help?
Chronic stress can make belly fat harder to lose — but supplements like ashwagandha, magnesium, and omega-3s may help restore cortisol balance. 🌿 Learn how science-backed nutrients support fat metabolism, calm your stress response, and bring your body back into harmony. ✨
-

How Ginseng Can Support Energy and Cortisol Balance
Ginseng is one of nature’s most powerful adaptogens, helping your body handle stress without burning out. 🌿 Learn how this ancient root supports balanced cortisol, steady energy, and sharper focus — restoring vitality naturally and sustainably. ✨
-

Taurine and Cortisol: Supporting Focus Under Stress
When cortisol surges, focus fades — but taurine helps restore balance. 🌿 Learn how this powerful amino acid calms your nervous system, regulates stress hormones, and sharpens concentration without jitters or fatigue. ✨
-
The Link Between Cortisol, Brain Fog, and Nutrient Deficiencies
When brain fog sets in, it’s not just in your head — it’s in your hormones. 🌿 Discover how cortisol imbalance and nutrient deficiencies like low magnesium, B vitamins, and omega-3s can cloud your focus and how restoring balance brings back mental clarity and calm. ✨
-

B Vitamins for Stress, Energy, and Cortisol Regulation
B vitamins are the foundation of stress resilience and steady energy. 🌿 Learn how this essential group of nutrients helps regulate cortisol, restore focus, and keep your nervous system calm — giving you balance from the inside out. ✨
-

Cortisol Imbalance and Chronic Fatigue: Can Supplements Help?
When chronic stress keeps cortisol high, fatigue and brain fog follow. 🌿 Learn how to rebalance your stress hormones naturally with calming nutrients, adaptogens, and lifestyle rituals that restore energy, focus, and inner peace. ✨
-

Adaptogen Stacks for Better Sleep and Lower Stress Hormones
Adaptogens can help your body recover from stress and sleep better by regulating key hormones like cortisol and adrenaline. 🌿 Learn how adaptogen stacks work to restore balance, calm the mind, and rebuild resilience — so you can rest deeply and wake renewed. ✨
-

Phosphatidylserine for Nighttime Cortisol Control
When stress hormones stay high at night, deep rest becomes impossible. 🌙 Discover how phosphatidylserine helps calm the brain, reduce nighttime cortisol, and restore healthy sleep rhythms — so you can wake up peaceful, clear, and recharged. ✨
-

Magnesium for Stress Relief and Cortisol Reduction
Magnesium is one of the most powerful natural tools for stress relief. 🌿 This essential mineral calms your nervous system, lowers cortisol, and helps your body recover from chronic tension. Learn how magnesium replenishes balance, improves sleep, and restores inner peace — naturally. ✨
-

Supplements to Improve Sleep by Balancing Cortisol
When cortisol stays high at night, sleep becomes a struggle. 🌙 Discover natural supplements that calm the nervous system, lower stress hormones, and restore your body’s natural rhythm. From magnesium and ashwagandha to L-theanine and phosphatidylserine, learn how to build deeper, more restorative rest. 🌿
-

Cortisol and Sleep: Why Stress Keeps You Awake
When stress keeps your body in fight-or-flight mode, cortisol refuses to calm down — and sleep becomes impossible. 🌙 Learn how elevated cortisol disrupts your circadian rhythm, suppresses melatonin, and turns restless nights into exhaustion. Discover how to restore balance and reclaim deep rest. ✨
-

L-Theanine for Cortisol Balance and Anxiety Relief
L-Theanine — the calming amino acid from green tea — helps quiet the mind and balance cortisol, the body’s key stress hormone. 🌿 Learn how it promotes calm focus, eases anxiety, and supports deep rest without sedation, backed by modern research and centuries of tradition. ✨
-

Rhodiola Rosea and Stress Resilience: A Natural Cortisol Regulator
Rhodiola rosea is one of nature’s most powerful tools for resilience. 🌿 This Arctic root helps balance cortisol, fight fatigue, and sharpen focus — keeping you calm yet energized even under stress. Discover the science behind Rhodiola’s adaptogenic power and how it helps your body thrive under pressure. ✨
-

Ashwagandha for Cortisol Balance: What the Science Says
Ashwagandha helps your body recover from chronic stress by calming the adrenal system and balancing cortisol — your key stress hormone. 🌿 Learn what science says about this powerful adaptogen, how it restores energy and focus, and why it’s one of nature’s most effective tools for modern stress relief. ✨
-

Supplements That Naturally Lower Cortisol Levels
When cortisol levels calm, your energy transforms — no more crashes or jitters, just steady focus and inner peace. 🌿 Learn which natural supplements and habits lower stress hormones, boost calm energy, and help your body thrive with balance instead of burnout. ✨
-

What Is Cortisol Imbalance? Symptoms You Shouldn’t Ignore
Cortisol — your body’s main stress hormone — keeps you alert and energized, but when it’s out of balance, it can drain your health. 🌿 Learn the signs of cortisol imbalance, from fatigue and anxiety to sleep disruption and stubborn weight gain, and discover how to restore calm, energy, and hormonal harmony naturally. ✨
-

The Best Daily Multivitamins for Menopausal Women
Menopause brings new nutritional needs that your old vitamin routine may no longer meet. 🌿 Discover how the right daily multivitamin can boost energy, balance mood, support bone and heart health, and keep your skin glowing. Learn which nutrients truly matter — from vitamin D to magnesium and B12 — to feel strong and vibrant every day. ✨
-

Antioxidants and Menopause: Fighting Inflammation Naturally
During menopause, oxidative stress and inflammation can quietly accelerate aging, fatigue, and skin changes. 🌿 Learn how antioxidants — from vitamins C and E to polyphenols in berries and green tea — help neutralize free radicals, reduce inflammation, and restore balance naturally. Discover the science of radiant, resilient aging. ✨
-

How CoQ10 Supports Heart Health After Menopause
After menopause, heart health becomes more important than ever. ❤️ Discover how CoQ10 — your body’s natural energy molecule — supports cardiovascular strength, restores vitality, and protects against oxidative stress. Learn how this essential nutrient helps keep your heart energized, balanced, and resilient through every stage of life. 🌿
-

Collagen Supplements for Skin and Joint Health Post-Menopause
After menopause, collagen loss affects both skin elasticity and joint comfort — but supplements can help rebuild from within. 🌸 Learn how collagen peptides, vitamin C, and other nutrients work together to restore firmness, reduce stiffness, and keep you glowing and mobile well into your next chapter. ✨
-

Calcium and Vitamin D: Protecting Bone Health in Menopause
Menopause brings hormonal changes that can weaken bones—but with the right nutrients, strength and stability can be rebuilt. 🦴 Learn how calcium and vitamin D work together to protect bone density, prevent fractures, and keep your body resilient. This guide explores nutrition, sunlight, and lifestyle habits that help your bones stay strong and vibrant for years to come. ☀️💪
-

Adaptogens for Energy and Resilience During Menopause
Feeling drained or emotionally scattered during menopause? 🌿 Discover how adaptogenic herbs like Ashwagandha, Rhodiola, and Ginseng can restore energy, balance cortisol, and build emotional resilience. Learn how these natural allies work with your body—not against it—to help you stay strong, focused, and calm through life’s hormonal changes. 🌸
-

Supplements That Help Beat Menopause Fatigue
Menopause fatigue can feel like more than tiredness—it’s a total energy crash. This guide explores how specific supplements, mindful breathwork, and therapy can help restore balance. Learn how nutrients like B vitamins, magnesium, and adaptogens rebuild your stamina, while breathwork and emotional healing calm your nervous system and bring vitality back to your days. 🌿✨
-

Herbal Blends for Menopausal Restlessness: Finding Calm in Transition
Herbal blends bring the wisdom of nature into moments of rest and renewal. Discover how soothing herbs like chamomile, lemon balm, and ashwagandha work together to calm menopausal restlessness, balance hormones, and invite deep relaxation. 🌿💫
-

Magnesium + Glycine for Deep Sleep During Menopause
Nutrients like magnesium, glycine, and B vitamins form the foundation for deep, restorative sleep during menopause. Discover how these natural compounds calm your nervous system, balance hormones, and help you wake up refreshed and recharged. 🌿💤
-

Melatonin and Menopause: Restoring Your Sleep Cycle
Nutrients are the foundation of hormone balance and energy. Learn how vitamins, minerals, and whole foods like greens, salmon, and berries nourish women’s bodies during menopause and beyond — restoring vitality, mood, and strength. 🌿🥗
-

How L-Theanine Helps With Menopausal Anxiety
Science continually deepens our understanding of the human body, from hormones to neurotransmitters. Discover how evidence-based research shapes modern wellness — bridging natural medicine, neuroscience, and hormone balance for healthier living. 🔬🌿
-

Can Ginkgo Biloba Improve Memory in Menopausal Women?
Hormone therapy can be a powerful tool for easing menopause symptoms and restoring balance. Learn how it works, the types available, and how to combine it safely with lifestyle and natural support for optimal well-being. 🌸💊
-

B Vitamins for Mental Clarity During Menopause
Nutrients are the foundation of mental and physical balance during menopause. Discover how vitamins, minerals, and whole foods like leafy greens, fish, nuts, and citrus can fuel energy, clarity, and calm while supporting hormonal health. 🌿✨
-

Mood Swings and Menopause: Natural Nutrient Support
Probiotics do more than support digestion — they help balance mood, hormones, and immunity too. Learn how a healthy gut microbiome can ease menopause symptoms, boost energy, and improve emotional resilience naturally. 🌿🦠
-

Brain Fog in Menopause: Supplements That May Help
Supplements can be powerful allies in restoring balance, energy, and focus—especially during menopause. Learn how nutrients like omega-3s, vitamin D, magnesium, and herbal adaptogens work together to support brain health, reduce stress, and promote lasting vitality. 🌿💊
-

Adaptogen Stacks for Reducing Night Sweats
Hormone detox isn’t about cleansing your body—it’s about restoring flow. Learn how the liver, gut, and endocrine systems work together to eliminate hormone buildup and how herbs like milk thistle, dandelion, and schisandra support balance, clarity, and natural vitality. 🌿💫
-

Cooling Menopause Symptoms with Herbal Support
Ashwagandha is one of nature’s most powerful adaptogens, helping women manage stress, sleep better, and balance hormones naturally. Discover how this ancient root supports calm energy, emotional resilience, and relief from menopause-related anxiety and fatigue. 🌿💫