The Risks and Benefits of Using Supplements Alongside BPD Medications
✨ Introduction
Borderline Personality Disorder (BPD) is a challenging condition marked by intense emotional swings 💔, impulsivity ⚡, unstable relationships 🤝, and a deep sensitivity to rejection 😢. For many people, medications—such as antidepressants, mood stabilizers, or antipsychotics—are part of treatment.
At the same time, a growing number of individuals with BPD are curious about supplements 🌱 to support emotional balance, reduce side effects, or improve overall well-being. But combining supplements with prescription medications can be a double-edged sword ⚔️.
This article explores both the potential benefits ✅ and possible risks ❌ of using supplements alongside BPD medications, while highlighting the importance of medical guidance, therapy, and a whole-person approach.
🧠 Medications Commonly Used in BPD
Unlike conditions such as bipolar disorder or depression, there is no single “BPD medication.” Instead, doctors may prescribe medications to target specific symptoms:
Antidepressants (SSRIs, SNRIs, TCAs) → reduce depressive moods and anxiety.
Mood stabilizers (lamotrigine, valproate, lithium) → address impulsivity and mood swings.
Antipsychotics (quetiapine, aripiprazole, risperidone) → help with paranoia, dissociation, or severe emotional dysregulation.
Anxiolytics (benzodiazepines, sometimes buspirone) → for short-term relief of acute anxiety.
Supplements can sometimes enhance these effects, but they can also interfere in dangerous ways.
✅ Potential Benefits of Supplements with BPD Medications

🌸 Filling Nutrient Gaps
Many psychiatric medications may deplete nutrients (e.g., folate, vitamin B12, magnesium, or CoQ10). Supplements can help restore balance and reduce fatigue, brain fog, or low mood.
Example:
SSRIs and SNRIs may lower B-vitamin levels → B-complex supplementation can help restore energy and mood.
⚖️ Supporting Emotional Regulation
Some supplements may complement medications by calming the nervous system or stabilizing mood:
Omega-3 fatty acids 🐟 → may reduce impulsivity and aggression.
Magnesium → calms overactive stress responses.
L-Theanine (from green tea 🍵) → promotes relaxation without sedation.
🌙 Improving Sleep
Insomnia is common in BPD, sometimes worsened by antidepressants or antipsychotics. Natural supports may help:
Melatonin → resets circadian rhythm.
Reishi mushroom 🍄 or Valerian root → promote deeper rest.
Looking for supplements for people with BPD? Click here.
🌿 Reducing Side Effects of Medications
Some supplements may counteract common medication side effects:
NAC (N-acetylcysteine) → may reduce irritability and cravings.
CoQ10 → combats fatigue linked to psychiatric medications.
🧘 Enhancing Therapy Engagement
When supplements reduce stress, improve sleep, or stabilize mood, people may be better able to focus on therapy 🛋️ (DBT, Schema Therapy, MBT). This integration is where supplements can make the biggest difference.
Looking for online therapy for people with BPD? Click Here.
⚠️ Risks of Mixing Supplements with BPD Medications
❌ Dangerous Interactions
Some supplements can dangerously amplify or reduce the effects of medications:
St. John’s Wort 🌼 → may interfere with SSRIs, risking serotonin syndrome (a potentially life-threatening condition).
5-HTP → when combined with antidepressants, can also cause serotonin syndrome.
Ginkgo Biloba 🍃 → may thin blood and increase bleeding risk when combined with antidepressants or mood stabilizers.
🚨 Worsening Side Effects
Supplements can intensify medication side effects:
Caffeine-based stimulants ☕ → can worsen anxiety and insomnia when taken with SSRIs.
High-dose Vitamin D → can cause calcium imbalances if combined with certain mood stabilizers.
⚖️ Overlapping Mechanisms
Some supplements act on the same neurotransmitters as medications. Doubling up can lead to excessive effects:
Ashwagandha 🌿 → while calming, can sometimes interact with sedatives, leading to too much drowsiness.
SAMe (S-adenosylmethionine) → boosts serotonin and dopamine but may destabilize mood when mixed with antidepressants.
🧩 Unpredictable Responses in BPD
People with BPD often have heightened sensitivity to emotional shifts. Supplements that cause even slight stimulation (Rhodiola, ginseng) can trigger agitation or impulsivity in some.
❌ Lack of Regulation
Supplements aren’t regulated like medications. Variability in purity, dosage, and contamination (e.g., heavy metals in herbs) can create risks, especially when mixed with prescription drugs.
🧠 The Role of Therapy Alongside Medications & Supplements

No supplement or medication can replace therapy for BPD. Evidence shows that Dialectical Behavior Therapy (DBT) remains the most effective intervention.
Supplements may:
🌬️ Reduce stress so mindfulness feels easier.
🛌 Improve sleep so emotional regulation skills are more accessible.
⚡ Stabilize mood enough to reduce impulsivity and engage in treatment.
But supplements should never be seen as substitutes for therapy—they are only adjunctive tools.
🌍 Lifestyle Foundations for Safe Supplement Use
To get the most from both medications and supplements, lifestyle practices are essential:
🧘 Breathwork & Meditation → regulate the nervous system.
Want to try Breathwork? Click Here.
🏋️ Exercise → improves mood and energy.
🥗 Balanced Diet → stabilizes blood sugar, reduces emotional crashes.
🌙 Sleep Hygiene → restores brain function.
💬 Therapeutic Support → ensures supplements are integrated safely.
🧾 Case Scenarios
Scenario 1: Supplements Help
Maria, diagnosed with BPD and on an SSRI, adds Omega-3s and magnesium with her doctor’s approval. Over time, her mood swings lessen, sleep improves, and she’s more engaged in DBT.
Scenario 2: Supplements Harm
Jake, also on an SSRI, self-starts St. John’s Wort after reading about its benefits. Within weeks, he develops agitation, tremors, and confusion—a classic case of serotonin syndrome.
👩 Key Safety Guidelines
Always consult your prescriber 👩⚕️ before adding supplements.
Introduce one supplement at a time → track reactions.
Start low, go slow ⏳ → BPD patients often have heightened sensitivity.
Avoid risky herbs like St. John’s Wort, 5-HTP, or kava unless supervised.
Choose high-quality brands with third-party testing.
Prioritize therapy and lifestyle—supplements are supportive, not replacements.
🌟 Conclusion
For people with Borderline Personality Disorder, supplements can be both helpers 🌱 and hazards ⚠️ when combined with medications. They may fill nutrient gaps, reduce side effects, and support therapy—but they can also trigger dangerous interactions or worsen instability.
The key is integration: supplements should only be used with medical oversight, therapeutic support, and lifestyle foundations in place. Done right, this combined approach can help those with BPD move toward greater resilience, stability, and hope 🌈.
📚 References
Linehan, M. (1993). Cognitive-Behavioral Treatment of Borderline Personality Disorder. Guilford Press.
Stoffers, J. M., et al. (2012). Psychological therapies for people with borderline personality disorder. Cochrane Database of Systematic Reviews.
Panossian, A., & Wikman, G. (2010). Effects of adaptogens on the central nervous system. Pharmaceuticals, 3(1), 188–224.
Mischoulon, D., & Fava, M. (2002). Role of S-adenosyl-L-methionine in the treatment of depression. CNS Drugs, 16(9), 671–681.
Sarris, J., et al. (2016). Adjunctive nutraceuticals for depression: a systematic review. American Journal of Psychiatry, 173(6), 575–587.
Related Posts
-

The Role of Omega-3s in Sleep Quality
-

Stacking GABA and Glycine for Deeper Rest
Discover how stacking GABA and glycine can help you achieve deeper, more restorative sleep. Learn how these calming amino acids work together to relax your mind, soothe your body, and improve overall sleep quality—naturally and safely.
-

Overcoming Jet Lag with Supplements
✈️ Jet lag doesn’t have to ruin your trip! Discover how supplements like melatonin, magnesium, L-theanine, and tart cherry can help you reset your body clock faster, reduce fatigue, and recover energy naturally after long flights. 🌙
-

Managing Sleep During Times of Stress
Feeling wired and restless? Learn how to manage sleep during stressful times through nutrition, breathwork, and natural supplements like magnesium and L-theanine. Discover how to calm your nervous system and restore deep, peaceful rest—even when life feels overwhelming.
-

The Role of Magnesium for Night Cramps
Night cramps keeping you awake? Discover how magnesium helps relax muscles, balance electrolytes, and prevent painful spasms. Learn which forms work best, how to take them, and how to pair them with other nutrients for cramp-free, peaceful sleep.
-

Supplements That Reduce Nighttime Awakenings
🌙 Discover science-backed supplements that help you stay asleep through the night. From magnesium and L-theanine to glycine and ashwagandha, learn how these natural compounds calm your nervous system, balance cortisol, and prevent 2 a.m. wake-ups for deeper, more restorative rest.
-

Nootropics That Promote Calm and Rest
Explore the world of calming nootropics — natural brain enhancers that promote relaxation, better focus, and deeper rest. Learn how L-Theanine, magnesium, ashwagandha, and other adaptogens help balance your nervous system, reduce stress, and support restorative sleep.
-

Best Natural Supplement Stack for Sleep
Discover the best natural supplement stack for deep, restorative sleep. Learn how nutrients like magnesium, L-theanine, glycine, and calming herbs such as chamomile and ashwagandha work together to relax your body, calm your mind, and improve sleep quality—naturally and safely.
-

Combining L-Theanine and Magnesium for Sleep: A Calm Night, Naturally
Discover how combining L-Theanine and Magnesium can help you drift into deep, restorative sleep. Learn how this natural duo calms the mind, relaxes the body, and supports your nervous system—without grogginess the next morning.
-

How to Sleep Better After Intense Workouts
Struggling to fall asleep after a tough workout? Learn how to optimize your post-training recovery with nutrition, hydration, and science-backed sleep strategies. Discover how to calm your nervous system, balance hormones, and wake up fully recharged for your next session.
-

Ashwagandha and Valerian: A Bedtime Combo for Deep Rest and Emotional Reset
Discover the calming synergy of Ashwagandha and Valerian root, two natural sleep aids that help quiet the mind, ease anxiety, and promote deeper rest. Learn how this herbal duo supports the nervous system, balances stress hormones, and restores emotional peace — without next-day grogginess.
-

How to Create a Resilience-Boosting Diet
Discover how to build emotional and physical strength from the inside out with a resilience-boosting diet 🍎. Learn which foods stabilize your mood, how supplements like magnesium and omega-3s strengthen your stress response, and why pairing nutrition with breathwork and therapy creates lasting calm, focus, and vitality 🌿💪.
-

Best Teas and Herbal Blends for Calmness: Nature’s Way to Restore Inner Peace
Ashwagandha, the ancient adaptogenic herb, helps your body find balance during stress. Known as “Indian ginseng,” it supports cortisol regulation, boosts energy, and restores calm clarity. Discover how this powerful root promotes resilience, emotional balance, and steady vitality — one cup at a time. 🌸
-

Parenting and Emotional Strength: How to Raise Children Without Losing Yourself
Empathy is the bridge that connects hearts — the quiet power to understand, feel, and support another’s emotions without judgment. Learn how empathy strengthens relationships, enhances communication, and cultivates deeper compassion in everyday life. 🌿
-
How to Bounce Back from Public Failure: Reclaiming Confidence, Purpose, and Power
Visualization is more than imagination — it’s brain training for resilience. By picturing calm, success, or healing, you activate the same neural pathways as real experience. Learn how daily visualization rewires your brain for confidence, emotional balance, and recovery from stress. ✨
-

Coping with Financial Stress Through Resilience: How to Stay Grounded When Money Feels Tight
Body awareness is the foundation of emotional resilience. By tuning into your body’s signals — tension, fatigue, or calm — you learn to recognize stress before it overwhelms you. Discover how mindfulness, gentle movement, and breathwork can deepen your connection with your body and restore balance from the inside out. 🧘
-

How to Stay Positive During Chronic Illness: A Guide to Emotional Strength and Hope
Creativity is more than art — it’s a form of healing. Whether through painting, writing, music, or small acts of expression, creativity helps release emotion, calm the nervous system, and reconnect you to joy. Discover how to use creativity as a tool for emotional balance, resilience, and self-discovery. 🌿
-

Resilience Tips for Caregivers: How to Stay Strong While Caring for Others
Joy isn’t the absence of pain — it’s the quiet strength to find light even in challenging times. Cultivating joy through small daily moments restores balance, releases stress, and reminds you of life’s beauty. Learn how to reconnect with authentic happiness, rebuild emotional energy, and nurture your nervous system through gratitude, presence, and play. 🌿
-

Building Resilience After a Breakup: How to Heal, Rebuild, and Rise Stronger
Social connection is one of the strongest predictors of emotional resilience. During difficult times, genuine relationships act as anchors — calming the nervous system, reducing stress hormones, and helping you regain perspective. Learn how cultivating real human connection can strengthen your mind, heart, and overall well-being. 🌿
-

How to Stay Emotionally Strong During Job Loss
Your emotions are powered by brain chemistry — a delicate balance of neurotransmitters like serotonin, dopamine, and cortisol. When these chemicals work in harmony, you feel calm, focused, and resilient. Learn how daily habits, nutrition, and mindfulness can support your brain chemistry and boost emotional well-being naturally. 🌿
-

The Role of Hormones in Emotional Stability: How Your Chemistry Shapes Your Calm
Hormones shape more than your body — they shape your emotions, resilience, and sense of calm. From cortisol to serotonin, these chemical messengers influence how you react to stress, connect with others, and recover from challenges. Learn how to balance your hormones naturally to build lasting emotional stability and harmony within. 💫
-

Mitochondria and Emotional Energy: The Cellular Power Behind Your Mood
Breathwork is one of the most powerful tools for emotional regulation and cellular balance. Through intentional breathing, you can calm your nervous system, increase oxygen flow to the brain, and even support mitochondrial energy. Learn how conscious breathing connects body and mind — transforming stress into presence and emotional strength. 🌿
-

Inflammation and Its Impact on Mood Resilience: The Silent Link Between Body and Mind
Inflammation doesn’t just affect the body — it impacts the mind. Chronic inflammation alters brain chemistry, depletes serotonin, and makes emotional recovery harder. Learn how calming inflammation through nutrition, mindfulness, and sleep can restore balance, resilience, and a renewed sense of emotional strength. 💫
-
How Antioxidants Protect Emotional Well-being: The Hidden Link Between Oxidative Stress and Mental Health
Antioxidants do more than protect your body — they defend your mind. By neutralizing oxidative stress, antioxidants support serotonin, dopamine, and brain energy pathways that keep you calm, focused, and emotionally balanced. Discover how foods like berries, green tea, and dark chocolate nourish your brain, boost mood, and strengthen resilience from the inside out. 🌿✨
-
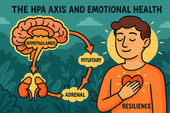
The HPA Axis and Emotional Health: The Hidden Bridge Between Stress and Mind
Neuroplasticity — the brain’s ability to rewire and adapt — is the foundation of emotional healing and resilience. When you face stress, trauma, or change, your neural pathways can reshape themselves to support new patterns of calm, focus, and self-awareness. Learn how daily practices like mindfulness, therapy, and breathwork strengthen neuroplasticity to transform emotional pain into personal growth. 🌸
-

Why Cortisol Control Is Key to Resilience: Mastering Stress to Build Emotional Strength
Controlling cortisol — the body’s main stress hormone — is the secret to lasting resilience. When cortisol levels stay balanced, your mind becomes clearer, emotions steadier, and energy more sustainable. Learn how breathwork, mindset shifts, adaptogens, and daily rhythms can help you calm your stress response and build true inner strength. 🌞💪
-
Dopamine’s Influence on Motivation and Recovery: Reigniting Drive and Balance
Healthy relationships are the foundation of emotional balance and resilience. Whether romantic, familial, or platonic, genuine connection releases dopamine, serotonin, and oxytocin — the brain’s “bonding trio” — helping us feel secure, motivated, and seen. Learn how trust, empathy, and communication not only strengthen your connections but also reshape your nervous system for deeper emotional well-being. 🌿🤝
-
The Role of Serotonin in Resilience: How This “Mood Molecule” Shapes Emotional Strength
Serotonin — often called the “resilience molecule” — plays a vital role in how we handle stress, regulate mood, and recover from emotional challenges. Beyond happiness, this powerful neurotransmitter helps balance the gut-brain axis, stabilize the nervous system, and support emotional flexibility. Learn how nutrition, sunlight, mindfulness, and adaptogens can naturally boost serotonin and strengthen your emotional resilience. 🌞🧠
-

How Neuroplasticity Supports Emotional Growth: Rewiring the Brain for Resilience
Neuroplasticity is the brain’s built-in power to grow, adapt, and heal — and it’s the foundation of emotional transformation. Every mindful breath, compassionate act, or reframed thought strengthens new neural pathways that support resilience and self-awareness. Learn how your brain rewires through daily habits, helping you turn emotional challenges into opportunities for growth and calm. 🌿
-

Tai Chi and Adaptogens for Mind-Body Balance: The Art of Harmonizing Energy and Resilience
Alchemy isn’t just an ancient science — it’s a timeless symbol of transformation and inner balance. By blending the physical and spiritual, alchemy teaches us that change begins from within. Just as metals are refined into gold, we too can transmute emotional pain, stress, and chaos into clarity and strength through mindful practice and self-awareness. 🌙✨
-

Cold Therapy and Emotional Control: Training the Mind Through the Body
Cold therapy isn’t just for athletes — it’s a tool for emotional mastery. By exposing your body to controlled cold, you train your nervous system to stay calm under stress, improving focus, mood, and resilience. This article explores the science of cold exposure, its impact on hormones and the vagus nerve, and how ice baths and cold showers can help you build emotional control, one breath at a time. 🧊🧘♂️
-

How Music Influences Emotional Recovery: The Healing Soundtrack of the Mind
Neuroplasticity — the brain’s ability to rewire and heal itself — is at the heart of emotional recovery. Through mindful habits, music, therapy, and consistent mental stimulation, your brain can form new connections that support resilience and well-being. Discover how neuroplasticity turns pain into growth, helping you rebuild balance, focus, and emotional strength. 🌿
-

Nature Therapy for Building Resilience: Reconnecting With the Healing Power of the Earth
Nature therapy helps rebuild emotional resilience by reconnecting you with the healing rhythms of the Earth. From forest walks to sunlight exposure, nature restores balance to your nervous system, lowers stress hormones, and teaches emotional adaptability. Learn how spending time outdoors can enhance mental clarity, calm anxiety, and awaken your natural capacity to heal. 🌞
-

Breathwork Techniques That Pair with Supplements: The Ultimate Synergy for Stress Relief and Mental Clarity
Breathwork and supplements create a powerful mind-body synergy for stress relief, focus, and energy. By combining intentional breathing with adaptogens, nootropics, and calming nutrients, you can naturally regulate cortisol, sharpen mental clarity, and boost emotional balance. This guide explores the best breathwork techniques and supplement pairings to help you feel centered, calm, and energized from the inside out. 🌿
-

Why Cortisol Balance Matters for Emotional Strength
Balancing cortisol — your body’s main stress hormone — is essential for emotional resilience. When cortisol is chronically high, your mind stays stuck in survival mode, leading to fatigue, anxiety, and emotional instability. This article explores how nutrition, supplements, breathwork, and therapy can help restore healthy cortisol rhythms, regulate the nervous system, and strengthen your ability to handle life’s challenges with calm focus and emotional strength. 🌿
-
Best Supplements for Students During Exam Season: Focus, Energy, and Memory Support
Studying late into the night? Learn which natural supplements can boost focus, memory, and mental stamina during exam season — without the crash. From omega-3s to Bacopa and Rhodiola, discover your brain’s ultimate exam support stack. 🎓🧠
-

Natural Memory Boosters for Seniors: How to Keep Your Mind Sharp and Focused
Stay mentally sharp and confident as you age. Discover science-backed natural supplements and lifestyle habits that boost memory, focus, and brain longevity for seniors. 🌿🧠
-
The Link Between Stress, Cortisol, and Memory Loss
Chronic stress can quietly erode your memory — and cortisol is the key culprit. Learn how stress hormones affect the brain, why the hippocampus shrinks under pressure, and how natural strategies can help you restore memory and mental clarity. 🧠✨
-

How to Build a Daily Supplement Routine for Memory Health
Want to sharpen your memory and stay mentally clear? Learn how to build a daily supplement routine for memory health — from morning focus to nighttime brain repair. Discover science-backed nutrients that boost recall, focus, and long-term cognitive resilience. 🧠🌿
-
Top 5 Natural Supplements for Memory Recall and Focus
Looking to boost memory and concentration naturally? Discover the top 5 supplements — Bacopa, Ginkgo Biloba, Lion’s Mane, Rhodiola, and Phosphatidylserine — that enhance focus, recall, and long-term brain health. 🧠✨
-

Top Supplements to Balance Mood Naturally
From omega-3s to adaptogens, discover the top natural supplements proven to support emotional balance, reduce stress, and promote inner calm — safely and effectively. 🌿✨
-

Can Omega-3 Fatty Acids Help with Mood Disorders?
Omega-3 fatty acids do more than support heart health — they can help balance mood, reduce depression, and calm anxiety. Discover how EPA and DHA nourish your brain, fight inflammation, and support emotional well-being from within. 🌊🧠
-

Vitamin D and Mood: The Sunshine Vitamin for Emotional Balance
Could the key to emotional balance be as simple as a little sunlight? Discover how vitamin D — the sunshine vitamin — influences serotonin, reduces inflammation, and helps you feel more positive and resilient year-round. ☀️💛
-

The Role of Magnesium in Reducing Irritability and Low Mood
Feeling on edge or emotionally drained? Magnesium could be the missing link between your body and your mood. Discover how this essential mineral reduces irritability, balances neurotransmitters, and helps your nervous system find calm again. 🌿✨
-
How Probiotics Influence Mood Through the Gut-Brain Axis
Discover how probiotics can do more than support your digestion—they can actually uplift your mood. This article explores the fascinating gut-brain axis and how balancing your gut bacteria through probiotics may help reduce anxiety, improve emotional stability, and support long-term mental well-being. 🌿🧠
-
Ashwagandha for Stress and Mood Regulation
Discover how Ashwagandha, the powerful adaptogenic herb 🌿, helps your body manage stress and regulate mood. Learn how it balances cortisol, boosts GABA and serotonin, and supports emotional stability — helping you feel calm, focused, and resilient every day.
-
St. John’s Wort: Natural Support for Mild to Moderate Depression
Discover how St. John’s Wort, the “sunshine herb” 🌼, naturally supports mild to moderate depression. Learn how it boosts serotonin, balances mood, and promotes emotional resilience — with research showing its effectiveness compares to antidepressants, but with fewer side effects.
-
Rhodiola Rosea and Mood Resilience Under Stress
Discover how Rhodiola rosea helps your body adapt to stress 🌿. Learn how this powerful adaptogen balances cortisol, supports serotonin and dopamine, and strengthens emotional resilience — helping you stay calm, focused, and energized under pressure.
-

Chamomile and Lavender: Herbal Calm for Emotional Fluctuations
Discover how chamomile and lavender bring calm to emotional ups and downs 🌿. Learn how these two soothing herbs balance your nervous system, ease anxiety, and support restful sleep — naturally helping you find peace and emotional stability.
-

Saffron Extract and Its Surprising Benefits for Mood Disorders
Discover how saffron extract — the golden spice of joy 🌸 — can naturally support mood balance, ease anxiety, and lift mild depression. Learn what science says about its serotonin-boosting power, the ideal dosage, and how this ancient remedy compares to modern antidepressants.