Inflammation and Its Impact on Mood Resilience: The Silent Link Between Body and Mind
Introduction
We often think of inflammation as something that happens when we sprain an ankle or fight off a cold. But what if the same biological process that heals your wounds could also quietly be shaping your mood, motivation, and mental strength?
Modern science has uncovered a fascinating truth: inflammation doesn’t stop at the body — it reaches the brain, influencing everything from how we handle stress to how resilient we feel after emotional setbacks.
When inflammation becomes chronic, it can sabotage the brain’s chemistry, dull motivation, and make emotional recovery harder. Yet by learning to reduce it — through diet, lifestyle, and mindset — we can unlock one of the most powerful tools for mood stability and resilience.
Let’s explore how inflammation affects your emotions, why it’s linked to anxiety and depression, and how to calm both body and mind from within. 🌸
Looking for supplements for Mood Resilience? Click here.
🔥 What Is Inflammation, Really?

Inflammation is the body’s natural defense mechanism. It’s how your immune system responds to injury, infection, or stress.
✅ Acute Inflammation
When you cut your finger or catch a virus, your immune system sends white blood cells and signaling molecules called cytokines to the site of damage. This causes redness, swelling, and heat — all signs that your body is healing.
⚠️ Chronic Inflammation
Problems arise when this process doesn’t shut off. Modern life — with its processed foods, stress, pollution, and sleep deprivation — keeps the immune system in a low-grade state of alert.
This “silent inflammation” doesn’t cause pain, but it slowly wears down tissues, blood vessels, and even neurons in your brain.
🧠 And because your brain and immune system are in constant communication, that low-level inflammation can profoundly influence your mood and mental resilience.
🧠 The Inflammatory Brain: How It Affects Mood
Your brain has its own immune cells, called microglia. When inflammation rises in the body, these cells become activated — releasing cytokines that affect neurotransmitters, neural plasticity, and hormone balance.
This creates what researchers call neuroinflammation — a state where the brain’s chemistry becomes cloudy and reactive.
🌩️ The Chain Reaction:
Inflammation increases cytokines like IL-6, TNF-alpha, and CRP.
These cytokines interfere with serotonin and dopamine production.
Energy levels drop, motivation wanes, and mood regulation falters.
Stress hormones like cortisol rise, perpetuating more inflammation.
The result? You feel drained, anxious, or flat — not because of weakness, but because your body’s biochemistry is inflamed.
“Inflammation doesn’t just make you tired — it makes your emotions tired too.” 🌿
💬 Mood Resilience: What It Means
Mood resilience isn’t about never feeling stressed or sad — it’s the ability to recover and return to balance.
It involves:
Emotional regulation 🧘
Cognitive flexibility 🧠
Physical energy 💪
Hormonal and neurotransmitter balance ⚖️
Inflammation disrupts all four of these pillars. That’s why chronic stress or poor diet can make emotional setbacks feel heavier or longer-lasting than they should.
Let’s look at exactly how.
⚡ The Inflammation–Depression Connection
For decades, depression was seen as a purely “chemical imbalance.” But today, scientists recognize inflammation as one of the most significant biological drivers of depressive symptoms.
🧬 The Cytokine Hypothesis of Depression
High levels of inflammatory cytokines — particularly IL-6, TNF-alpha, and CRP — have been consistently linked to depression and low mood.
These cytokines:
Reduce serotonin availability (the “calm and contentment” neurotransmitter).
Impair dopamine signaling, lowering motivation and pleasure.
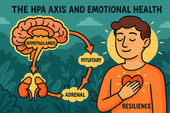
Activate the HPA axis, increasing cortisol and anxiety.
Decrease neurogenesis (the creation of new brain cells), leading to emotional rigidity.
Even inflammation from infections or autoimmune disorders can trigger depressive symptoms — showing how deeply connected mood and immunity truly are.
🧠 In simple terms: inflammation makes the brain less flexible, and resilience depends on flexibility.
🌩️ Inflammation and Anxiety
Anxiety often coexists with inflammation. Studies show that elevated cytokines can increase amygdala activity — the brain’s fear center — making you more reactive to stress.
Chronic inflammation also alters gut-brain signaling, leading to restlessness, irritability, or physical symptoms like a racing heart.
Interestingly, anti-inflammatory interventions — like omega-3 supplementation or mindfulness — often reduce both inflammation and anxiety levels.
🌿 When the body cools, the mind calms.
🌿 How Inflammation Weakens Emotional Recovery
After a stressful event, your body should shift from fight-or-flight to rest-and-repair mode. But if inflammation is high, this transition gets stuck.
Cortisol stays elevated.
Sleep becomes shallow.
The nervous system remains on alert.
Emotional processing feels harder.
Essentially, inflammation “locks” the stress response in place, preventing full recovery.
That’s why people under chronic inflammation often feel emotionally fatigued — as if their stress never truly ends.
💞 The Gut–Brain Axis: Where Inflammation Begins
Over 70% of your immune system resides in your gut, where trillions of microbes (the microbiome) interact with your nervous system and HPA axis.
When the gut barrier becomes compromised — a condition often called “leaky gut” — inflammatory molecules enter the bloodstream, affecting the brain.
This process can lower serotonin (since much of it is made in the gut) and increase anxiety.
Key triggers include:
Processed foods 🍟
Excess sugar 🍬
Alcohol and antibiotics 🍷💊
Chronic stress 😣
🦠 A calm gut equals a calm brain.
🧘 Inflammation, Neuroplasticity, and Emotional Resilience
Resilience depends on neuroplasticity — your brain’s ability to form new connections and learn from experience.
Inflammation suppresses BDNF (Brain-Derived Neurotrophic Factor) — a protein essential for neuroplasticity and emotional healing.
When BDNF levels drop, it becomes harder to adapt, learn, and recover emotionally.
Antioxidants, exercise, and mindfulness all increase BDNF, helping reverse this inflammatory rigidity.
🌸 Neuroplasticity is emotional flexibility at the molecular level.
🌾 Signs Your Mood May Be Affected by Inflammation
Constant fatigue or “brain fog”
Heightened reactivity to stress
Trouble sleeping or waking unrefreshed
Digestive discomfort (bloating, irregularity)
Joint pain or stiffness
Low motivation or apathy
Feeling “emotionally heavy” without clear cause
These are not just “mood” symptoms — they’re body–mind feedback loops showing inflammation’s reach.
🧃 Anti-Inflammatory Nutrients for Mood Balance
Food is the fastest way to influence inflammation — for better or worse. Here are key nutrients that calm inflammation and support emotional health:
🐟 Omega-3 Fatty Acids (EPA & DHA)
Reduce inflammatory cytokines, improve serotonin signaling, and protect neurons.
Sources: salmon, sardines, chia, flax, algae oil.
🌿 Curcumin (from Turmeric)
Blocks NF-kB, a key inflammatory pathway linked to mood disorders.
Tip: Combine with black pepper for 2000% better absorption.
🍇 Polyphenols
Found in berries, green tea, olive oil, and dark chocolate — they reduce oxidative stress and boost BDNF.
🥦 Sulforaphane
A compound in cruciferous vegetables that activates the body’s detox and anti-inflammatory genes.
🧄 N-Acetyl Cysteine (NAC)
Boosts glutathione, the master antioxidant, and reduces neuroinflammation — shown in studies to support mood recovery.
🍊 Vitamin C & E
These antioxidants reduce cortisol levels and protect brain cells from inflammatory damage.
Looking for supplements for Mood Resilience? Click here.
🧘 Lifestyle Habits to Lower Inflammation and Strengthen Resilience
🌤️ Prioritize Deep, Restful Sleep
Poor sleep raises inflammation and weakens mood regulation.
Try consistent bedtimes, dark rooms, and digital cutoffs an hour before bed.
💨 Practice Breathwork and Mindfulness
Slow, deep breathing lowers cytokines and cortisol.
Mindfulness meditation has been shown to reduce CRP (C-reactive protein) levels — a key inflammatory marker.
🪷 A calm breath is anti-inflammatory medicine.
Want to try Breathwork? Click Here.
🏃 Move Daily
Exercise releases anti-inflammatory myokines and boosts dopamine and serotonin.
Even brisk walking 30 minutes a day can shift your inflammatory profile toward healing.
🌸 Manage Psychological Stress
Stress is one of the strongest triggers of inflammation.
Therapies like CBT, journaling, and grounding techniques calm both the brain and immune system.
Looking for online therapy ? Click Here.
🥗 Eat Whole, Colorful Foods
Each color in plants represents different antioxidants — together they form your emotional armor.
Avoid refined carbs, excess oils, and processed meats.
🫶 Foster Connection and Compassion
Social isolation increases inflammation and weakens immunity.
Acts of kindness and community bonding, conversely, reduce inflammatory gene expression.
💞 Love is literal medicine.
🌿 Supplements That Support Anti-Inflammatory Mood
| Supplement | Key Benefit | Evidence |
|---|---|---|
| Omega-3 (EPA) | Lowers inflammation, improves mood | Strong clinical support |
| Curcumin | Blocks inflammatory pathways | Shown to reduce depression symptoms |
| NAC | Boosts glutathione, neuroprotection | Used in mood disorder trials |
| Vitamin D3 | Immune modulation, serotonin regulation | Deficiency linked to depression |
| Magnesium Glycinate | Calms HPA axis, reduces stress | Widely studied |
| Probiotics (Lactobacillus, Bifidobacterium) | Gut–brain balance | Improves mood and stress resilience |
Always consult a healthcare professional before starting new supplements, especially if taking medications. 🌱
💫 The Mind–Body Dialogue: Emotional Healing as Inflammatory Healing
When inflammation cools, your emotions regain clarity.
That’s because your body and mind are in constant dialogue:
The immune system influences your thoughts.
The gut sends signals of safety or danger to the brain.
Every emotion you feel changes your body’s biochemistry.
By reducing inflammation, you restore that dialogue to harmony.
🌿 Emotional resilience is not about ignoring pain — it’s about giving your biology room to heal.
🌻 Integrating Anti-Inflammatory Living
Here’s how to bring it all together into your day:
🌅 Morning
Hydrate with lemon water (vitamin C).
Get 10 minutes of sunlight exposure.
Eat a protein-rich, colorful breakfast.
☀️ Afternoon
Move your body — even short walks lower inflammatory markers.
Snack on berries or nuts.
Take 5 minutes to breathe deeply or stretch.
🌙 Evening
Disconnect from screens an hour before bed.
Eat an anti-inflammatory dinner (salmon, greens, olive oil).
Reflect or journal gratitude to calm stress chemistry.
💬 These small rituals, repeated daily, shift your immune response from fight to flow.
🧬 Inflammation, Trauma, and Emotional Sensitivity

People with a history of trauma often show higher inflammation markers.
That’s because trauma sensitizes both the nervous system and immune system, making the body more reactive to stress.
Healing requires both psychological and biological repair. Practices like:
Somatic therapy (body-based emotional release),
EMDR, and
Breath-centered meditation
…help deactivate the body’s alarm systems, calming both inflammation and emotional hypervigilance.
🪷 You can’t think your way out of inflammation — but you can feel your way into balance.
🌞 The Positive Side: Anti-Inflammatory Emotions
Not all inflammation comes from food or stress — emotions themselves can shift inflammation up or down.
Studies show that emotions like gratitude, compassion, and joy lower pro-inflammatory cytokines.
Meanwhile, rumination, resentment, and loneliness raise them.
💗 Practicing positive emotions is not “toxic positivity” — it’s immunological resilience.
“What you hold in your heart shapes what flows through your blood.” 🌸
🌺 Emotional Resilience as an Anti-Inflammatory Skill
When you strengthen emotional resilience, you indirectly lower inflammation.
You regulate your stress response, improve sleep, and reduce cytokine signaling.
Likewise, when you cool inflammation, your emotional range expands — joy, calm, and focus come back online.
The two are inseparable:
Emotional healing lowers inflammation.
Biological healing improves emotion.
🧘 Resilience is both mindset and chemistry.
🌿 Final Thoughts: Cooling the Fire Within
Inflammation is not your enemy — it’s your body’s way of saying, “Something needs healing.”
But when it becomes chronic, it blocks the very systems that keep you strong and emotionally adaptable.
By nourishing your cells with antioxidants, calming your breath, sleeping deeply, and choosing anti-inflammatory foods, you’re not just protecting your heart or brain — you’re healing your mood at the molecular level.
“When the body is inflamed, the mind burns out.
When the body cools, the heart remembers how to hope.” 🌿💫
Resilience isn’t found in avoiding stress — it’s built by keeping your internal fire steady and clear.
📚 References
Dantzer, R. et al. (2008). From inflammation to sickness and depression: When the immune system subjugates the brain. Nature Reviews Neuroscience.
Miller, A. H., & Raison, C. L. (2016). The role of inflammation in depression: From evolutionary imperative to modern treatment target. Nature Reviews Immunology.
Berk, M. et al. (2013). Inflammation and oxidative stress in mood disorders: A pathway to treatment. Biological Psychiatry.
Haroon, E., Raison, C. L., & Miller, A. H. (2012). Psychoneuroimmunology and the role of cytokines in mood regulation. Molecular Psychiatry.
Kiecolt-Glaser, J. K. et al. (2015). Mindfulness meditation and reduced inflammation. Psychosomatic Medicine.
Felger, J. C. (2018). Inflammation, fatigue, and motivation: A neuroimmune perspective. Trends in Neurosciences.
Slavich, G. M., & Irwin, M. R. (2014). From stress to inflammation and depression: Linking psychological and biological processes. Annual Review of Clinical Psychology.
Ng, F. et al. (2008). The role of nutrition and inflammation in mental health. Journal of Affective Disorders.
Panossian, A., & Wikman, G. (2010). Adaptogens and stress protection. Pharmaceuticals.
Maes, M. et al. (2021). The inflammatory theory of depression: Revisited. Frontiers in Psychiatry.
Related Posts
-

Nootropics That Promote Calm and Rest
Explore the world of calming nootropics — natural brain enhancers that promote relaxation, better focus, and deeper rest. Learn how L-Theanine, magnesium, ashwagandha, and other adaptogens help balance your nervous system, reduce stress, and support restorative sleep.
-

Best Natural Supplement Stack for Sleep
Discover the best natural supplement stack for deep, restorative sleep. Learn how nutrients like magnesium, L-theanine, glycine, and calming herbs such as chamomile and ashwagandha work together to relax your body, calm your mind, and improve sleep quality—naturally and safely.
-

Combining L-Theanine and Magnesium for Sleep: A Calm Night, Naturally
Discover how combining L-Theanine and Magnesium can help you drift into deep, restorative sleep. Learn how this natural duo calms the mind, relaxes the body, and supports your nervous system—without grogginess the next morning.
-

How to Sleep Better After Intense Workouts
Struggling to fall asleep after a tough workout? Learn how to optimize your post-training recovery with nutrition, hydration, and science-backed sleep strategies. Discover how to calm your nervous system, balance hormones, and wake up fully recharged for your next session.
-

Ashwagandha and Valerian: A Bedtime Combo for Deep Rest and Emotional Reset
Discover the calming synergy of Ashwagandha and Valerian root, two natural sleep aids that help quiet the mind, ease anxiety, and promote deeper rest. Learn how this herbal duo supports the nervous system, balances stress hormones, and restores emotional peace — without next-day grogginess.
-

How to Create a Resilience-Boosting Diet
Discover how to build emotional and physical strength from the inside out with a resilience-boosting diet 🍎. Learn which foods stabilize your mood, how supplements like magnesium and omega-3s strengthen your stress response, and why pairing nutrition with breathwork and therapy creates lasting calm, focus, and vitality 🌿💪.
-

Best Teas and Herbal Blends for Calmness: Nature’s Way to Restore Inner Peace
Ashwagandha, the ancient adaptogenic herb, helps your body find balance during stress. Known as “Indian ginseng,” it supports cortisol regulation, boosts energy, and restores calm clarity. Discover how this powerful root promotes resilience, emotional balance, and steady vitality — one cup at a time. 🌸
-

Parenting and Emotional Strength: How to Raise Children Without Losing Yourself
Empathy is the bridge that connects hearts — the quiet power to understand, feel, and support another’s emotions without judgment. Learn how empathy strengthens relationships, enhances communication, and cultivates deeper compassion in everyday life. 🌿
-
How to Bounce Back from Public Failure: Reclaiming Confidence, Purpose, and Power
Visualization is more than imagination — it’s brain training for resilience. By picturing calm, success, or healing, you activate the same neural pathways as real experience. Learn how daily visualization rewires your brain for confidence, emotional balance, and recovery from stress. ✨
-

Coping with Financial Stress Through Resilience: How to Stay Grounded When Money Feels Tight
Body awareness is the foundation of emotional resilience. By tuning into your body’s signals — tension, fatigue, or calm — you learn to recognize stress before it overwhelms you. Discover how mindfulness, gentle movement, and breathwork can deepen your connection with your body and restore balance from the inside out. 🧘
-

How to Stay Positive During Chronic Illness: A Guide to Emotional Strength and Hope
Creativity is more than art — it’s a form of healing. Whether through painting, writing, music, or small acts of expression, creativity helps release emotion, calm the nervous system, and reconnect you to joy. Discover how to use creativity as a tool for emotional balance, resilience, and self-discovery. 🌿
-

Resilience Tips for Caregivers: How to Stay Strong While Caring for Others
Joy isn’t the absence of pain — it’s the quiet strength to find light even in challenging times. Cultivating joy through small daily moments restores balance, releases stress, and reminds you of life’s beauty. Learn how to reconnect with authentic happiness, rebuild emotional energy, and nurture your nervous system through gratitude, presence, and play. 🌿
-

Building Resilience After a Breakup: How to Heal, Rebuild, and Rise Stronger
Social connection is one of the strongest predictors of emotional resilience. During difficult times, genuine relationships act as anchors — calming the nervous system, reducing stress hormones, and helping you regain perspective. Learn how cultivating real human connection can strengthen your mind, heart, and overall well-being. 🌿
-

How to Stay Emotionally Strong During Job Loss
Your emotions are powered by brain chemistry — a delicate balance of neurotransmitters like serotonin, dopamine, and cortisol. When these chemicals work in harmony, you feel calm, focused, and resilient. Learn how daily habits, nutrition, and mindfulness can support your brain chemistry and boost emotional well-being naturally. 🌿
-

The Role of Hormones in Emotional Stability: How Your Chemistry Shapes Your Calm
Hormones shape more than your body — they shape your emotions, resilience, and sense of calm. From cortisol to serotonin, these chemical messengers influence how you react to stress, connect with others, and recover from challenges. Learn how to balance your hormones naturally to build lasting emotional stability and harmony within. 💫
-

Mitochondria and Emotional Energy: The Cellular Power Behind Your Mood
Breathwork is one of the most powerful tools for emotional regulation and cellular balance. Through intentional breathing, you can calm your nervous system, increase oxygen flow to the brain, and even support mitochondrial energy. Learn how conscious breathing connects body and mind — transforming stress into presence and emotional strength. 🌿
-
How Antioxidants Protect Emotional Well-being: The Hidden Link Between Oxidative Stress and Mental Health
Antioxidants do more than protect your body — they defend your mind. By neutralizing oxidative stress, antioxidants support serotonin, dopamine, and brain energy pathways that keep you calm, focused, and emotionally balanced. Discover how foods like berries, green tea, and dark chocolate nourish your brain, boost mood, and strengthen resilience from the inside out. 🌿✨
-
The HPA Axis and Emotional Health: The Hidden Bridge Between Stress and Mind
Neuroplasticity — the brain’s ability to rewire and adapt — is the foundation of emotional healing and resilience. When you face stress, trauma, or change, your neural pathways can reshape themselves to support new patterns of calm, focus, and self-awareness. Learn how daily practices like mindfulness, therapy, and breathwork strengthen neuroplasticity to transform emotional pain into personal growth. 🌸
-

Why Cortisol Control Is Key to Resilience: Mastering Stress to Build Emotional Strength
Controlling cortisol — the body’s main stress hormone — is the secret to lasting resilience. When cortisol levels stay balanced, your mind becomes clearer, emotions steadier, and energy more sustainable. Learn how breathwork, mindset shifts, adaptogens, and daily rhythms can help you calm your stress response and build true inner strength. 🌞💪
-
Dopamine’s Influence on Motivation and Recovery: Reigniting Drive and Balance
Healthy relationships are the foundation of emotional balance and resilience. Whether romantic, familial, or platonic, genuine connection releases dopamine, serotonin, and oxytocin — the brain’s “bonding trio” — helping us feel secure, motivated, and seen. Learn how trust, empathy, and communication not only strengthen your connections but also reshape your nervous system for deeper emotional well-being. 🌿🤝
-
The Role of Serotonin in Resilience: How This “Mood Molecule” Shapes Emotional Strength
Serotonin — often called the “resilience molecule” — plays a vital role in how we handle stress, regulate mood, and recover from emotional challenges. Beyond happiness, this powerful neurotransmitter helps balance the gut-brain axis, stabilize the nervous system, and support emotional flexibility. Learn how nutrition, sunlight, mindfulness, and adaptogens can naturally boost serotonin and strengthen your emotional resilience. 🌞🧠
-

How Neuroplasticity Supports Emotional Growth: Rewiring the Brain for Resilience
Neuroplasticity is the brain’s built-in power to grow, adapt, and heal — and it’s the foundation of emotional transformation. Every mindful breath, compassionate act, or reframed thought strengthens new neural pathways that support resilience and self-awareness. Learn how your brain rewires through daily habits, helping you turn emotional challenges into opportunities for growth and calm. 🌿
-

Tai Chi and Adaptogens for Mind-Body Balance: The Art of Harmonizing Energy and Resilience
Alchemy isn’t just an ancient science — it’s a timeless symbol of transformation and inner balance. By blending the physical and spiritual, alchemy teaches us that change begins from within. Just as metals are refined into gold, we too can transmute emotional pain, stress, and chaos into clarity and strength through mindful practice and self-awareness. 🌙✨
-

Cold Therapy and Emotional Control: Training the Mind Through the Body
Cold therapy isn’t just for athletes — it’s a tool for emotional mastery. By exposing your body to controlled cold, you train your nervous system to stay calm under stress, improving focus, mood, and resilience. This article explores the science of cold exposure, its impact on hormones and the vagus nerve, and how ice baths and cold showers can help you build emotional control, one breath at a time. 🧊🧘♂️
-

How Music Influences Emotional Recovery: The Healing Soundtrack of the Mind
Neuroplasticity — the brain’s ability to rewire and heal itself — is at the heart of emotional recovery. Through mindful habits, music, therapy, and consistent mental stimulation, your brain can form new connections that support resilience and well-being. Discover how neuroplasticity turns pain into growth, helping you rebuild balance, focus, and emotional strength. 🌿
-

Nature Therapy for Building Resilience: Reconnecting With the Healing Power of the Earth
Nature therapy helps rebuild emotional resilience by reconnecting you with the healing rhythms of the Earth. From forest walks to sunlight exposure, nature restores balance to your nervous system, lowers stress hormones, and teaches emotional adaptability. Learn how spending time outdoors can enhance mental clarity, calm anxiety, and awaken your natural capacity to heal. 🌞
-

Breathwork Techniques That Pair with Supplements: The Ultimate Synergy for Stress Relief and Mental Clarity
Breathwork and supplements create a powerful mind-body synergy for stress relief, focus, and energy. By combining intentional breathing with adaptogens, nootropics, and calming nutrients, you can naturally regulate cortisol, sharpen mental clarity, and boost emotional balance. This guide explores the best breathwork techniques and supplement pairings to help you feel centered, calm, and energized from the inside out. 🌿
-

Why Cortisol Balance Matters for Emotional Strength
Balancing cortisol — your body’s main stress hormone — is essential for emotional resilience. When cortisol is chronically high, your mind stays stuck in survival mode, leading to fatigue, anxiety, and emotional instability. This article explores how nutrition, supplements, breathwork, and therapy can help restore healthy cortisol rhythms, regulate the nervous system, and strengthen your ability to handle life’s challenges with calm focus and emotional strength. 🌿
-
Best Supplements for Students During Exam Season: Focus, Energy, and Memory Support
Studying late into the night? Learn which natural supplements can boost focus, memory, and mental stamina during exam season — without the crash. From omega-3s to Bacopa and Rhodiola, discover your brain’s ultimate exam support stack. 🎓🧠
-

Natural Memory Boosters for Seniors: How to Keep Your Mind Sharp and Focused
Stay mentally sharp and confident as you age. Discover science-backed natural supplements and lifestyle habits that boost memory, focus, and brain longevity for seniors. 🌿🧠
-
The Link Between Stress, Cortisol, and Memory Loss
Chronic stress can quietly erode your memory — and cortisol is the key culprit. Learn how stress hormones affect the brain, why the hippocampus shrinks under pressure, and how natural strategies can help you restore memory and mental clarity. 🧠✨
-

How to Build a Daily Supplement Routine for Memory Health
Want to sharpen your memory and stay mentally clear? Learn how to build a daily supplement routine for memory health — from morning focus to nighttime brain repair. Discover science-backed nutrients that boost recall, focus, and long-term cognitive resilience. 🧠🌿
-
Top 5 Natural Supplements for Memory Recall and Focus
Looking to boost memory and concentration naturally? Discover the top 5 supplements — Bacopa, Ginkgo Biloba, Lion’s Mane, Rhodiola, and Phosphatidylserine — that enhance focus, recall, and long-term brain health. 🧠✨
-

Top Supplements to Balance Mood Naturally
From omega-3s to adaptogens, discover the top natural supplements proven to support emotional balance, reduce stress, and promote inner calm — safely and effectively. 🌿✨
-

Can Omega-3 Fatty Acids Help with Mood Disorders?
Omega-3 fatty acids do more than support heart health — they can help balance mood, reduce depression, and calm anxiety. Discover how EPA and DHA nourish your brain, fight inflammation, and support emotional well-being from within. 🌊🧠
-

Vitamin D and Mood: The Sunshine Vitamin for Emotional Balance
Could the key to emotional balance be as simple as a little sunlight? Discover how vitamin D — the sunshine vitamin — influences serotonin, reduces inflammation, and helps you feel more positive and resilient year-round. ☀️💛
-

The Role of Magnesium in Reducing Irritability and Low Mood
Feeling on edge or emotionally drained? Magnesium could be the missing link between your body and your mood. Discover how this essential mineral reduces irritability, balances neurotransmitters, and helps your nervous system find calm again. 🌿✨
-
How Probiotics Influence Mood Through the Gut-Brain Axis
Discover how probiotics can do more than support your digestion—they can actually uplift your mood. This article explores the fascinating gut-brain axis and how balancing your gut bacteria through probiotics may help reduce anxiety, improve emotional stability, and support long-term mental well-being. 🌿🧠
-
Ashwagandha for Stress and Mood Regulation
Discover how Ashwagandha, the powerful adaptogenic herb 🌿, helps your body manage stress and regulate mood. Learn how it balances cortisol, boosts GABA and serotonin, and supports emotional stability — helping you feel calm, focused, and resilient every day.
-
St. John’s Wort: Natural Support for Mild to Moderate Depression
Discover how St. John’s Wort, the “sunshine herb” 🌼, naturally supports mild to moderate depression. Learn how it boosts serotonin, balances mood, and promotes emotional resilience — with research showing its effectiveness compares to antidepressants, but with fewer side effects.
-
Rhodiola Rosea and Mood Resilience Under Stress
Discover how Rhodiola rosea helps your body adapt to stress 🌿. Learn how this powerful adaptogen balances cortisol, supports serotonin and dopamine, and strengthens emotional resilience — helping you stay calm, focused, and energized under pressure.
-

Chamomile and Lavender: Herbal Calm for Emotional Fluctuations
Discover how chamomile and lavender bring calm to emotional ups and downs 🌿. Learn how these two soothing herbs balance your nervous system, ease anxiety, and support restful sleep — naturally helping you find peace and emotional stability.
-

Saffron Extract and Its Surprising Benefits for Mood Disorders
Discover how saffron extract — the golden spice of joy 🌸 — can naturally support mood balance, ease anxiety, and lift mild depression. Learn what science says about its serotonin-boosting power, the ideal dosage, and how this ancient remedy compares to modern antidepressants.
-

5-HTP and Serotonin: A Natural Path to Lifting Mood
Discover how 5-HTP naturally boosts serotonin 🌞 — the neurotransmitter behind mood, sleep, and emotional balance. Learn how this plant-derived compound supports happiness, reduces anxiety, and improves rest by helping your brain create more serotonin the gentle, natural way.
-
GABA Supplements for Reducing Anxiety and Mood Swings
Discover how GABA supplements can help reduce anxiety and balance mood naturally 🌿. Learn how this calming neurotransmitter works to quiet the mind, ease stress, and improve sleep — plus which nutrients and habits can boost your body’s own GABA production for long-term emotional stability.
-
L-Theanine for Calm Focus and Mood Stability
Discover how L-theanine, the calming compound found in green tea 🍵, promotes focus, relaxation, and mood stability. Learn the science behind how it balances neurotransmitters, reduces stress hormones, and enhances clarity — helping you stay centered, calm, and productive without sedation.
-

B Vitamins and Brain Chemistry: Supporting Energy and Emotional Balance
Discover how B vitamins power your brain chemistry ⚡. Learn how B6, B9, and B12 support serotonin, dopamine, and energy production — helping boost focus, mood, and emotional balance. From diet to supplements, explore how this vital nutrient group keeps your mind resilient and your energy steady.
-

N-Acetyl Cysteine (NAC) and Mood Disorders: What the Research Says
Learn how N-Acetyl Cysteine (NAC) supports brain health and mood balance 🧠. Discover how this antioxidant helps reduce oxidative stress, regulate glutamate, and improve emotional stability in depression, bipolar disorder, and anxiety — backed by cutting-edge psychiatric research.
-

Supplements for Bipolar Disorder: What May Support Stability
Discover the best supplements for bipolar disorder 🌿 that may support emotional stability and brain health. Learn how nutrients like omega-3s, magnesium, vitamin D, and NAC can help reduce inflammation, balance neurotransmitters, and complement traditional treatment safely.